The endocrine system and the human system
For an organism to function normally and effectively, it is necessary that the biochemical processes of its tissues operate smoothly and conjointly in a stable setting. The endocrine system provides an essential mechanism called homeostasis that integrates body activities and at the same time ensures that the composition of the body fluids bathing the constituent cells remains constant.
Scientists have postulated that the concentrations of the various salts present in the fluids of the body closely resemble the concentrations of salts in the primordial seas, which nourished the simple organisms from which increasingly complex species have evolved. Any change in the salt composition of fluids that surround cells, such as the extracellular fluid and the fluid portion of the circulating blood (the serum), necessitates large compensating changes in the salt concentrations within cells. As a result, the constancy of these salts ( electrolytes) inside and outside of cells is closely guarded. Even small changes in the serum concentrations of these electrolytes (e.g., sodium, potassium, chloride, calcium, magnesium, and phosphate) elicit prompt responses from the endocrine system in order to restore normal concentrations. These responses are initiated through negative feedback regulatory mechanisms similar to those described above.
Not only is the concentration of each individual electrolyte maintained through homeostasis, but the total concentration of all of the electrolytes per unit of fluid (osmolality) is maintained as well. If this were not the case, an increase in extracellular osmolality (an increase in the concentrations of electrolytes outside of cells) would result in the movement of intracellular fluid across the cell membrane into the extracellular fluid. Because the kidneys would excrete much of the fluid from the expanded extracellular volume, dehydration would occur. Conversely, decreased serum osmolality (a decrease in the concentrations of electrolytes outside of cells) would lead to a buildup of fluid within the cells.
Another homeostatic mechanism involves the maintenance of plasma volume. If the total volume of fluid within the circulation increases (overhydration), the pressure against the walls of the blood vessels and the heart increases, stimulating sensitive areas in heart and vessel walls to release hormones. These hormones, called natriuretic hormones, increase the excretion of water and electrolytes by the kidney, thus reducing the plasma volume to normal.
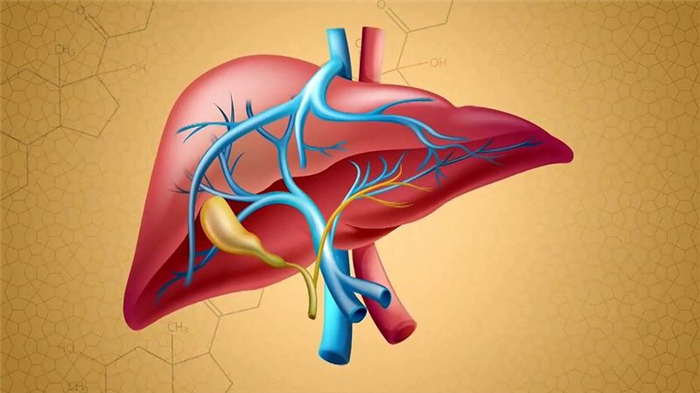
Hormonal systems also provide for the homeostasis of nutrients and fuels that are needed for body metabolism. For example, the blood glucose concentration is closely regulated by several hormones to ensure that glucose is available when needed and stored when in abundance. After food is ingested, increased blood glucose concentrations stimulate the secretion of insulin. Insulin then stimulates the uptake of glucose by muscle tissue and adipose tissue and inhibits the production of glucose by the liver. In contrast, during fasting, blood glucose concentrations and insulin secretion decrease, thereby increasing glucose production by the liver and decreasing glucose uptake by muscle tissue and adipose tissue and preventing greater reductions in blood glucose concentrations.
Growth and differentiation
Despite the many mechanisms designed to maintain a constant internal environment, the organism itself is subject to change: it is born, it matures, and it ages. These changes are accompanied by many changes in the composition of body fluids and tissues. For example, the serum phosphate concentration in healthy children ranges from about 4 to 7 mg per 100 ml (1.1 to 2.1 millimole per litre [mmol/l]), whereas the concentration in normal adults ranges from about 3 to 4.5 mg per 100 ml (1 to 1.3 mmol/l). These and other more striking changes are part of a second major function of the endocrine system—namely, the control of growth and development. The mammalian fetus develops in the uterus of the mother in a system known as the fetoplacental unit. In this system the fetus is under the powerful influence of hormones from its own endocrine glands and hormones produced by the mother and the placenta. Maternal endocrine glands assure that a proper mixture of nutrients is transferred by way of the placenta to the growing fetus. Hormones also are present in the mother’s milk and are transferred to the suckling young.
Sexual differentiation of the fetus into a male or a female is also controlled by delicately timed hormonal changes. Following birth and a period of steady growth in infancy and childhood, the changes associated with puberty and adolescence take place. This dramatic transformation of an adolescent into a physically mature adult is also initiated and controlled by the endocrine system. In addition, the process of aging and senescence in adults is associated with endocrine-related changes.
Adaptive responses to stress
Throughout life the endocrine system and the hormones it secretes enhance the ability of the body to respond to stressful internal and external stimuli. The endocrine system allows not only the individual organism but also the species to survive. Acutely threatened animals and humans respond to stress with multiple physical changes, including endocrine changes, that prepare them to react or retreat. This process is known as the “ fight-or-flight” response. Endocrine changes associated with this response include increased secretion of cortisol by the adrenal cortex, increased secretion of glucagon by the islet cells of the pancreas, and increased secretion of epinephrine and norepinephrine by the adrenal medulla.
Adaptive responses to more prolonged stresses also occur. For example, in states of starvation or malnutrition, there is reduced production of thyroid hormone, leading to a lower metabolic rate. A low metabolic rate reduces the rate of the consumption of the body’s fuel and thus reduces the rate of consumption of the remaining energy stores. This change has obvious survival value since death from starvation is deferred. Malnutrition also causes a decrease in the production of gonadotropins and sex steroids, reducing the need for fuel to support reproductive processes.