The Anatomy of the Pineal Gland
Deep within the brain is the tiny pineal gland, an organ that produces the body’s melatonin, an influential hormone that helps to regulate sleep and wakefulness and the circadian patterns that have broad effects on health. Discover more about the anatomy, location, and function of the pineal body and how it influences sleep, affects seasonal reproduction in animals, and may be impacted by specific brain tumors.
Anatomy
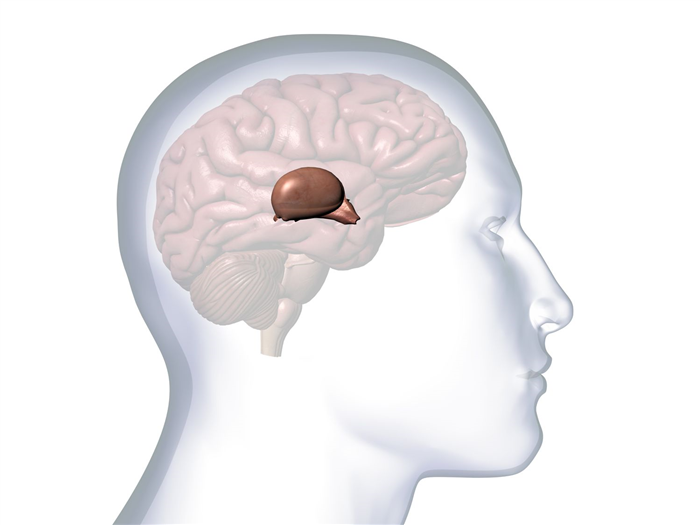
The pineal gland (or pineal body) is a small, pine-cone shaped organ that lies within the roof of the third ventricle, deep within the brain. Autopsy studies have shown that the average size of the pineal gland is similar to that of a grain of rice. The ventricles are fluid-filled spaces, and the third ventricle extends from the large lateral ventricles to the narrow cerebral aqueduct, passing between the two halves of the part of the brain called the diencephalon.
It is located within an area called the epithalamus, just behind the thalamus and above the cerebellum, resting at the back of the brain, near the brain stem. There is a small fluid-filled pineal recess that projects into the stalk of the pineal body, allowing for the hormones it produces to more easily be diffused throughout the brain.
Structure
The cells that make up the tissue of the pineal gland in humans and other mammals include hormone-producing pinealocytes and the supportive interstitial cells. Nerve cells, or neurons, might influence the pinealocytes by secreting specific chemicals called neurotransmitters. Nerve fibers reach the gland via the pineal stalk and contain many substances, including:
The pinealocyte cells have receptors for all these neurotransmitters, suggesting influence from these other chemicals that are common within the brain.
In humans and other mammals, this influence is extended beyond the brain to a collection of neurons located in the sympathetic superior cervical ganglia and the parasympathetic sphenopalatine and otic ganglia. This connection is a relay from the pineal gland to the suprachiasmatic nucleus (SCN), located in the hypothalamus.
The SCN is of vital importance because this is the primary pacemaker for the circadian rhythm within the body, affected by the perception of light detected by the retina and sent along the retinohypothalamic tract.
Function
The most important function of the pineal gland is the production of melatonin. Melatonin is synthesized from molecules of the neurotransmitter serotonin. Once produced, it is secreted from the pineal gland. It has important effects on circadian rhythm, including impacts on sleep and possible effects on seasonal reproduction in animals.
Within the pineal gland, serotonin (which is derived from the amino acid called tryptophan) undergoes a transformation, when an acetyl group and then a methyl group are added to yield melatonin. This is accomplished with two enzymes: serotonin-N-acetyltransferase and hydroxyindole-O-methyltranferase. The production of melatonin is impaired by light exposure.
How does light affect melatonin production within the pineal gland? In order to answer this question, it is important to understand how light generally affects the circadian rhythms of the body.
From the Latin meaning “about a day,” the word “circadian” refers to numerous physiological processes that are coupled to the timing of light and darkness. Though inclusive of sleep and wakefulness, this circadian timing likely extends to the release of hormones, the use of energy to optimize metabolism, and the coordination of the body’s interconnected systems.
Light that passes through the retina of the eye activates specific receptors called intrinsically photosensitive retinal ganglion cells (ipRGC). These cells contain the photopigment called melanopsin. From here, the signal is relayed from the eyes to the pineal gland.
First, the message is passed along the retinohypothalamic tract that extends from the retinal cells to the SCN in the anterior hypothalamus in the brain. The paraventricular nucleus of the hypothalamus then sends the signal along to the preganglionic sympathetic neurons in the spinal cord, to the superior cervical ganglion, and finally on to the pineal gland.
The pineal gland can then alter its production of melatonin, based on the amount of light that is perceived by the eyes. This has led the pineal gland to be called the “third eye” of the body, due to its ability to respond to the perception of light.
When melatonin is produced, it is not released into a vacuum to do as it pleases. As is true for many processes within the body, there is a balance that is preserved. This balance is called homeostasis. When the pineal gland secretes melatonin, this feeds back via action on the MT1 and MT2 melatonin receptors on the SCN. This interplay affects the control of the circadian system within the body, with broader implications for potential disease.
There are a few other curious effects of melatonin that are not fully understood within humans. It is known that in animal models melatonin can decrease gonadotropin-releasing hormone (GnRH) secretion from the hypothalamus. This may have an inhibitory effect on reproductive functions. In mammals, this may slow the maturation of sperm and eggs and reduce the function of the reproductive organs.
It is theorized that it may affect the seasonal reproductive functions of some animals. When nights are longer in the winter months, and the access to food may be reduced, the increased darkness may lead to higher melatonin levels and reduced fertility. This may make it less likely for some animal species to have young that may not survive the lean times of winter. The significance of this, especially among humans, is unknown.
There is some caution advised in the use of supplemental melatonin (which is the only unregulated hormone available for purchase over the counter in the United States) in pregnant women and children, however. The release of melatonin by the pineal gland may play a role in the timing of human sexual maturation. Melatonin levels decline slightly at puberty, and pineal tumors that eliminate melatonin production will cause premature puberty in young children.
Finally, melatonin produced by the pineal gland is a very effective antioxidant. It may protect neurons within the central nervous system from free radicals, such as nitric oxide or hydrogen peroxide. These chemicals are generated in active neural tissues. Free radicals may increase the risk of tissue damage and dysfunction, including the risk for medical problems like cancer and neurodegenerative disease.
It is also known that melatonin production decreases with natural aging, and how this exacerbates disease is still being investigated.
Associated Conditions
The pineal gland and its production of melatonin are central to the circadian rhythm disorders that affect sleep. It may exacerbate insomnia in delayed sleep phase syndrome, for example. It also may have a role in seasonal affective disorder, sometimes known as winter depression. In addition, when the pineal gland is affected by tumors, the effects may lead to brain surgery.
Circadian Rhythm Disorders
These conditions occur when the synchrony between the patterns of wakefulness and sleep do not align with societal norms or the natural rhythm of light and darkness. Characterized by irregular bedtimes and awakenings, the affected person will experience insomnia and improperly timed sleepiness. The circadian sleep disorders include:
- Delayed sleep phase syndrome: Night owls who have difficulty getting to sleep and trouble waking at an early time
- Advanced sleep phase syndrome: Characterized by early sleep onset and early morning awakening
- Free-running, or non-24: Most often found in blind people without light perception, the timing of sleep may shift gradually over weeks or months
- Irregular sleep-wake rhythm: Shorter intervals of sleep over the 24-hour day, rather than a prolonged sleep period overnight
How can the timing of sleep be disordered? Ultimately, this may depend on personal perspective, largely influenced by social context. One must be careful to avoid labeling normal variations of physiologic patterns as a disease. When there is significant social and occupational dysfunction (including absenteeism from school or work), treatment may be appropriate. Fortunately, for those whose irregular sleep patterns are without consequence, medical help is not typically sought.
Seasonal Affective Disorder (SAD)
With the prolonged darkness of night that occurs in the winter months within the northern hemisphere, seasonal affective disorder may ensue. Also known as winter depression, the condition may be associated with other symptoms, including reduced physical activity and weight gain.
Phototherapy, with the artificial application of light from a light box or light therapy glasses, may be helpful. The timing of the light is typically in the morning, but it is important to follow the guidance of a medical professional.
Pineal Gland Tumors
Cancer may rarely affect the pineal gland. In fact, less than 1 percent of brain tumors occur in the pineal gland, but 3%–8% of brain tumors in children are found here. Generally, pineal gland tumors occur more among young adults, those individuals between 20 and 40 years of age. There are only a handful of tumors that may affect the pineal gland within the brain. In fact, there are only three types of true pineal cell tumors. These include:
- Pineocytoma: Slow growing, often classified as a grade II tumor
- Pineoblastoma: Generally more aggressive, either classified as a grade III intermediate form or more malignant grade IV
- Mixed pineal tumor: Contains a combination of cell types, making a clean classification less possible
These tumors may grow large enough to obstruct the normal flow of the cerebrospinal fluid within the ventricles. It is estimated that 10%–20% of the pineal gland tumors may also spread via this medium, especially the more aggressive pineoblastoma variant. Fortunately, these cancers rarely metastasize elsewhere in the body.
Symptoms that develop with a pineal gland tumor may include:
If a pineal gland tumor is identified, treatment typically includes radiation. If pineoblastoma is present, the entire brain and spinal cord must receive radiation therapy. If the tumor has spread, or if it regrows after radiation treatment, chemotherapy may be indicated. In some cases, surgery may be done to determine the tumor type by removing part of the tumor. If the flow of cerebrospinal fluid is blocked, leading to swelling within the brain, a shunt may be placed to ensure normal circulation beyond the site of the tumor.
Other Conditions
It is notable that certain medications may affect the relay from the eye’s perception of light to the production of melatonin within the pineal gland. In particular, beta-blocking medications that are used to treat hypertension, tachycardia, and heart disease may interfere with the normal release of melatonin. Beta-blockers include Lopressor (metoprolol), Tenormin (atenolol), and Inderal (propranolol). If this has significant impacts on sleep or health, a different medication may need to be used.
The pineal gland may become calcified in older individuals, lighting up on computed tomography (CT) scans due to their increased density, and leading to the presence of “brain sand” on a pathological assessment of the tissue.
Tests
In most cases, testing to assess the pineal gland is not indicated. Melatonin levels can be measured in the saliva, blood, and urine without direct assessment of the pineal gland; however, this is mostly done in context of research studies and not in clinical care. Given its size, some imaging techniques may provide only limited data about the structure. In the context of pineal gland tumors, the following tests may be appropriate:
Further assessment of the circadian disorders may require evaluation by a board-certified sleep specialist who will ask targeted questions to further understand the patterns and impacts of the problem.
Tracking of the circadian rhythm may be done longitudinally with sleep logs or actigraphy. Wearable technology, including common fitness trackers, may provide some of this biometric data. The sleep specialist will also direct appropriate interventions, including the potential use of melatonin supplementation or phototherapy, to optimize sleep and well-being.
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- Boafo A, Greenham S, Alenezi S, et al. Could long-term administration of melatonin to prepubertal children affect timing of puberty? A clinician’s perspective. Nat Sci Sleep. 2019;11:1–10. Published 2019 Jan 31. doi:10.2147/NSS.S181365
- American Brain Tumor Association. Pineal tumors.
- Scheer FA, Morris CJ, Garcia JI, et al. Repeated melatonin supplementation improves sleep in hypertensive patients treated with beta-blockers: a randomized controlled trial. Sleep. 2012;35(10):1395–1402. Published 2012 Oct 1. doi:10.5665/sleep.2122
- Tan DX, Xu B, Zhou X, Reiter RJ. Pineal calcification, melatonin production, aging, associated health consequences and rejuvenation of the pineal gland. Molecules. 2018;23(2):301. Published 2018 Jan 31. doi:10.3390/molecules23020301
- Erlich SS and ML Apuzzo. The pineal gland: anatomy, physiology, and clinical significance. J Neurosurg. 1985 Sep;63(3):321-41. doi:10.3171/jns.1985.63.3.0321.
- Macchi MM and JN Bruce. Human pineal physiology and functional significance of melatonin. Front Neuroendocrinol. 2004 Sep-Dec;25(3-4):177-95. doi:10.1016/j.yfrne.2004.08.001.
- Martini FH. Fundamentals of Anatomy & Physiology. Prentice Hall, New Jersey, 4th edition, p. 628.
- Moller M and FM Baeres. The anatomy and innervation of the mammalian pineal gland. Cell Tissue Res. 2002 Jul;309(1):139-50. Epub 2002 May 18. doi:10.1007/s00441-002-0580-5.
By Brandon Peters, MD
Brandon Peters, MD, is a board-certified neurologist and sleep medicine specialist.