15 Endocrine system
No cell is an island. With the emergence of multi-cellular organisms appeared a need for communication between cells to coordinate the activities of specialized tissues for the benefit of an entire organism. The endocrine system plays a major role in this process.
Now, we know that practically every organ sends signals (hormones) to other body parts to elicit biological responses that adjust the behavior of these target organs to maintain homeostasis. The heart does it, fat does it, as do the stomach and intestines. However, this chapter covers only the glandular organs that secrete hormones as their primary function.
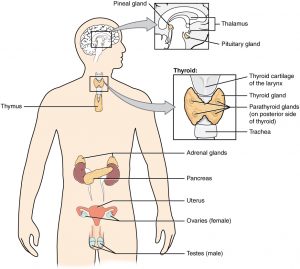
The “classic” endocrine glands in the human body include the pituitary, thyroid, parathyroid, adrenal
and pineal glands. Some other glands with endocrine cells have both endocrine and non-endocrine functions. The pancreas is one of these glands, where the non-endocrine function is secreting digestive enzymes to the small intestine.
The diagram below shows the endocrine glands and their localization throughout the body. The pineal gland and the pituitary gland are located in the brain. The thyroid gland, located within the neck, wraps around the trachea. Four small, disc-shaped parathyroid glands are embedded into the posterior side of the thyroid. The adrenal glands are located on top of each kidney. The pancreas is located in the upper portion of the abdomen. In females, the two ovaries are in the pelvic cavity, while in males, the two testes are located in the scrotum.
Pituitary
The human pituitary gland is a small endocrine gland attached to the inferior surface of the brain by a thin thread of tissue called the infundibulum. The pituitary has two parts or lobes, the anterior pituitary (a.k.a adenohypophysis) and a posterior pituitary (a.k.a neurohypophysis.) The two parts of the pituitary have different origins, are made of different tissues and look different under the microscope. Both parts have a fairly rich network of sinusoid capillaries that pick up secreted hormones.
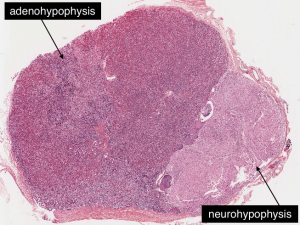 |
Anterior pituitary
The anterior lobe is made of secretory epithelial cells and can be recognized by the presence of glandular epithelium. The hormone-secreting cells are arranged along the sinusoidal capillaries into cords sharply outlined by collagenous fibers.
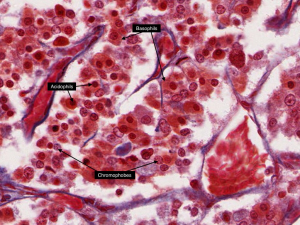
The pituitary is frequently stained with more than hematoxylin-eosin in order to show the different types of hormone-secreting cells. The colors of the cells depend on the hormones the cell produces and stores in the secretory granules. In Masson’s trichrome stain:
The acidophils are dark red and rounded. They include cells that produce growth hormone (GH) and prolactin.
The basophils are blue and produce luteinizing hormone (LH), follicle stimulating hormone (FSH), thyroid stimulating hormone (TSH) and adrenal cortical stimulating hormone (ACTH).
The chromophobes are light orange or faded and are ACTH producing cells, or cells that have emptied their granules.
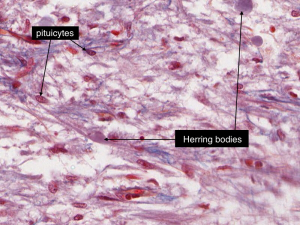
Hypothalamus and posterior pituitary
The posterior lobe is made of the axons of hypothalamic neurons extending through the infundibulum, and pituicytes, which are the specialized glial cells. In the trichrome stain, the posterior lobe looks grayish and vacuolated. The large magenta-stained swellings are Herring bodies, the secretory granules containing either oxytocin or anti-diuretic hormone (ADH). The red-pink nuclei belong to pituicytes.
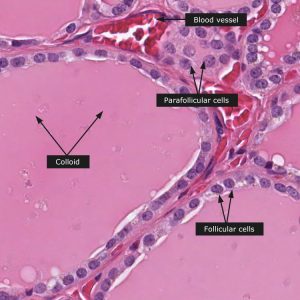
Thyroid gland
The majority of the thyroid gland is made of spherical structures called follicles, instead of cords and clusters characteristic of the endocrine system. The central cavity of a follicle is filled with a colloid composed of thyroglobulin. Thyroglobulin is a glycoprotein that is a precursor and storage molecule for thyroid hormones. An extensive network of capillaries around follicles allows for the easy pick up of hormones by the blood.
The thyroid gland has two types of endocrine cells with different functions.
Follicular cells are the secretory (glandular) epithelial cells surrounding a cavity filled with a pink thyroglobulin. The height of the follicular cells reflects the functional state of the thyroid. The more active the cells, the taller the follicular cells. Follicular cells with normal activity are simple cuboidal; the highly active cells become columnar, the inactive cells flatten to squamous. Follicular cells produce and secrete the hormones thyroxine and triiodothyronine.
The parafollicular cells are primarily located in clusters between follicles but can also be a part of the follicular wall. Parafollicular cells are larger, oval in shape and have lighter stained cytoplasm than follicular cells. These cells secrete calcitonin.
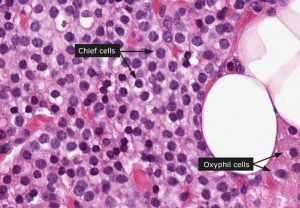
Parathyroid glands
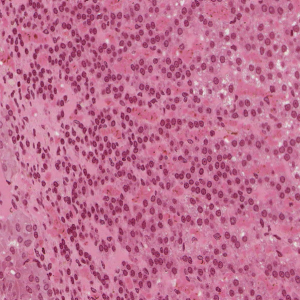
Parathyroid glands are small glands located on the posterior side of the thyroid. There are two types of cells in the parathyroid glands, chief cells, that secrete hormones and non-secreting oxyphil cells.
The majority of the cells are chief cells. They have clear cytoplasm and small, centrally placed, round nuclei. Cells are arranged into cords of cells surrounded by sinusoidal capillaries. Oxyphil cells are larger and intensely eosinophilic (pink) and may be found interspersed or in clusters among the chief cells. The function of the oxyphil cells is unknown.
Adrenal glands
The adrenal gland is another “double origin” and double function endocrine organ. The outside layer of the triangle-shaped organ, the cortex, is made of the steroid hormone producing cells, and secretes cortisol, aldosterone and adrenal androgens. In the interior is a medulla that is part of the autonomic nervous system, and is made of the chromaffin cells that secrete catecholamines, adrenaline and noradrenaline. The adrenal gland is covered by an outer connective tissue capsule. In the center of the adrenal gland lies the large central vein.
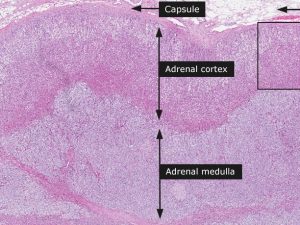
Adrenal cortex
Going from outside, from the connective tissue capsule, the adrenal cortex is comprised of three distinctly recognizable layers:
-
- a thin zona glomerulosa
- a wide zona fasciculata
- a thin zona reticularis
The cells of the zona glomerulosa are small, with round nuclei and arranged in loops and arcades. This layer is darker in appearance due to the closely located nuclei.
The cells of zona fasciculata are large and are arranged into columns. The nuclei are round and larger than those of the zona glomerulosa or zona reticularis. The accumulation of lipid droplets in the cytoplasm of these cells (white spots in histological preps) gives this zone a vacuolated appearance.
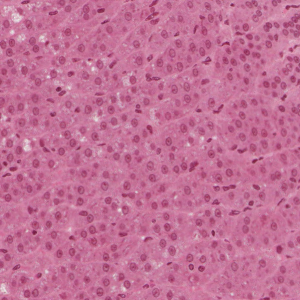
The cells of zona reticularis are smaller than those of the zona fasciculata and look like a branched network. The cytoplasm may contain brown pigment and gives this zone a darker appearance. Zona reticularis borders the medulla on the inside.
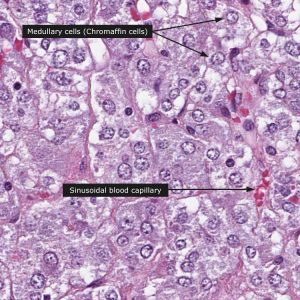
Adrenal medulla
The medulla is composed of the chromaffin cells that are arranged in cords and clumps surrounded by sinusoidal capillaries. The chromaffin cells have a clear cytoplasm in hematoxylin/eosin staining, but after dichromate fixation they can appear brown due to the oxidation of the catecholamines with dichromate salts. Cells making norepinephrine stain darker than those making epinephrine.
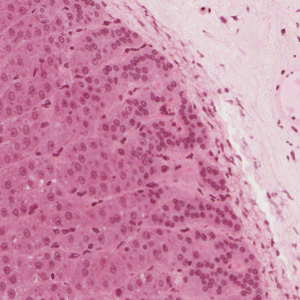
Endocrine Pancreas
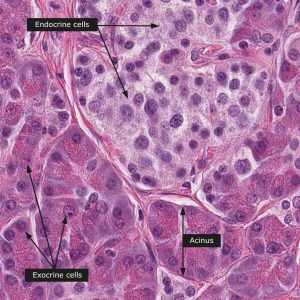
Pancreas has both exocrine and endocrine components. The endocrine component of the pancreas consists of the islets of Langerhans, the round masses of glandular epithelial cells appearing as nodules in the endocrine pancreas. The cells are found in irregular cords and clumps, as opposed to the neighboring, highly organized acini of the exocrine pancreas. They are surrounded by a network of capillaries. Two principal cells in the islets are the alpha cells that secrete glucagon, and the beta cells that secrete insulin. These cell types cannot be differentiated by light microscopy, and biopsy is of no use in diagnosing type 1 diabetes.
License
Histology Copyright © by Malgosia Wilk-Blaszczak. All Rights Reserved.