Structure and function of the sweat glands
The sweat glands are exocrine glands distributed throughout the body surface. They are sometimes referred to as sudoriferous or sudoriparous glands. These names are derived from the latin word ‘sudor’ which means ‘sweat’. There are two types of sweat glands:
- Eccrine glands are found all over the body and secrete a watery product that cools the skin.
- Apocrine sweat glands are mainly found in the armpits and perianal area, and secrete a more viscous, odorous product.
There are several histological differences between these two types of glands, but they do share a common general structure. That is, they both consist of a secretory and duct (excretory) segments.
This article will discuss the histology and functions of the sweat glands.
| Definition | Exocrine glands that produce sweat, located within the dermis/subcutis of the skin. |
| Types | Eccrine glands Apocrine glands |
| Eccrine glands | Simple coiled glands whose watery excretion aids thermoregulation by evaporating from the body surface, thus cooling the body. |
| Apocrine glands | Simple tubular glands whose excretion contributes to body odor. |
Basic structure
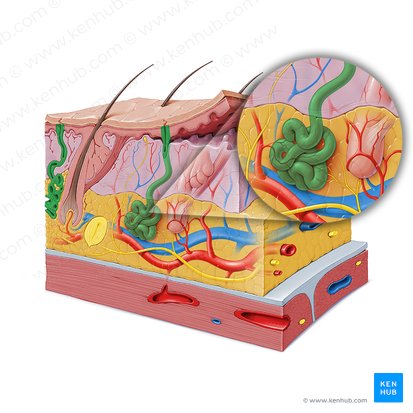
In general, sweat glands tend to comprise a secretory unit which is located either in the deep dermis or in the subcutaneous tissue, and a duct which continues from the secretory unit towards the body surface, through which sweat or secretory product is passed.
The secretory units of sweat glands are surrounded by contractile myoepithelial cells which act to help secrete the gland’s product. The contraction of these cells are either controlled by hormones or nerve action.
Sweat glands open into the skin’s surface, or in the case of apocrine sweat glands, into hair follicles. The part of the gland that opens onto the skin or hair follicle is known as the acrosyringium. Whilst sweat glands share a basic structure, apocrine and eccrine sweat glands have many differences which are outlined during the rest of this article.
Eccrine sweat glands
The eccrine glands are simple coiled glands whose main function is to help in regulating the temperature of the body. They secrete hypotonic solution, i.e. the sweat, whose evaporation helps cooling the body. In the process of producing the sweat, the eccrine glands reabsorb a certain amount of sodium and water, which is why the sweat is hypotonic. With sweat, we excrete ammonia, urea, uric acid and sodium chloride.
In contrast to the apocrine glands, the eccrine glands are not related to the hair follicle, but instead exist as independent structures located in the skin of the whole body, except for the lips and external genitals.
Eccrine glands consist of two segments: secretory and duct. The secretory segment is found in the deep dermis or in the superficial part of the subcutaneous tissue. The duct segment is continuous with the secretory, coiling from it towards the surface of the skin.
Secretory segment
The secretory segment consists of three types of cells that lie on the basal lamina: clear, dark and myoepithelial. The clear and dark cells are the secretory cells, while the myoepithelial are the contractile cells. Given the different sizes of cells, the lining of the secretory segment resembles to the pseudostratified epithelium.
- The clear cells contain large amounts of glycogen, numerous smooth endoplasmic reticula and mitochondria, as well as a small Golgi apparatus. The function of these cells is to produce the electrolytes watery component of sweat.
- The dark cells contain numerous rough endoplasmic reticula and a well-developed Golgi apparatus. This is because they produce the glycoprotein component of the sweat. These components are packed within secretory granules which are usually found aggregated in the apical cytoplasm.
- The myoepithelial cells are contractile cells, usually dispersed between the clear and dark cells. They are filled with contractile filaments and their contraction promotes fast excretion of sweat.
Duct segment
The duct segment continues from the secretory segment and goes towards the skin surface. After leaving the dermis, it exhibits slight coiling in course. It is lined by the stratified cuboidal epithelium which has two layers: basal or peripheral layer which is deep, and luminal or apical layer which lies on top of the basal layer. It is important to note that the duct segment does not contain myoepithelial cells.
The basal cells have an ellipsoid nucleus with a prominent nucleolus, as well as a large amount of ribosomes and mitochondria. The luminal cells have smaller nucleus than basal. Their most distinguishing feature is the presence of glassy or hyalinized structure in their cytoplasm, which represents accumulated tonofilaments.
Function
The eccrine glands are responsible for thermoregulatory sweating. Simply said, when the ambient temperature is too high, these glands release sweat which then evaporates and conveys the heat from the body. This type of physiological sweating first starts in the skin of the scalp and forehead, then to the face and the rest of the skin. The last regions to exhibit the thermoregulatory sweating are palms and soles.
In contrast to thermoregulatory sweating, there is also sweating induced by the emotional stress. In this situation, the palms, soles and axillae are the first regions to sweat.
The nervous stimulation for thermoregulatory and stress sweating is different. The thermoregulatory sweating is stimulated by the cholinergic input, whereas the stress sweating is promoted by the adrenergic input.
Apocrine sweat glands
The apocrine glands are coiled tubular sweat glands associated with the hair follicles of the skin. They are found in the skin of axilla, areola, nipples, perianal skin and the skin of external genitals.
The apocrine glands secrete a viscous, oily substance, that is yellow in color, and has an acrid odor. This secretion is produced in response to the presence of bacterial decomposition. Apocrine sweat glands are controlled by sex hormones and therefore only become active at puberty. In contrast to the eccrine glands, there is no reabsorption or any modification of the excretory product whatsoever in the apocrine glands.
They also consist of a secretory and a duct segments.
Secretory segment
The secretory portion is usually located in the superficial layer of the subcutis, however it can sometimes be found in the deep dermis. There are a couple of histological characteristics which differ the secretory segment of apocrine glands from that of the eccrine glands:
- The secretory part of apocrine glands is much wider than that of the eccrine glands.
- The apocrine glands store their product in their lumina, while as we noted before, the eccrine glands store them in the granules within the apical cytoplasm of their cells.
The secretory segment of apocrine glands is lined by simple epithelium which consists of only one cell type. These cells appear eosinophilic and they feature a protrusion on their apical region. It was believed that the separation of this protrusion from the cell is the mechanism of excretion of cellular product. This is why the glands bear the name apocrine, derived from the word apex which means “the tip”, suggesting that the pinching of the tip is the way of excretion. However, recent studies have proven that this is not true. Instead, the cells pack their products in small granules, which then reach the lumen through the process of exocytosis. This way of secretion is called merocrine secretion.
The cells are also rich in lysosomes, mitochondria and lipofuscin and feature a prominent Golgi apparatus, especially when the secretion phase is active.
Myoepithelial cells are also dispersed throughout the lining of the secretory segment. Their function is to aid excretion with their contractions.
Duct segment
The duct of apocrine glands has a narrow lumen and a relatively straight course towards the hair follicle where it opens. It is lined by the stratified cuboidal epithelium which is devoid of myoepithelial cells.
The epithelium usually consists of 2-3 cell layers. The cells of the luminal layer, which is the most superficial one, contain glassy aggregation in their apical cytoplasm, which, similar to that of eccrine glands, represents the aggregation of tonofilaments.
Functions
The activity of the apocrine glands heavily depends on sex hormones. In other mammals, these glands release a significant amount of pheromones which affects the odour and ‘chemical fingerprint’ of an animal. It is considered that the odour plays an important role in sexual pairing and social treatment of an animal.
Although in humans the product of apocrine glands also affects the body odor, its social and sexual significance is consider as rudimentary to non-existent.
Clinical notes
Sweat gland dysfunction can lead to a variety of abnormalities and diseases. For example, inflammation of the apocrine sweat glands can lead to the rare diseases known as Fox-Fordyce disease. This causes a persistent rash in the pubic regions and armpits, and is more common in women. Moreover, if the eccrine glands become exhausted due to excessive activity, this can contribute to heatstroke. This in turn can result in hyperpyrexia, which is categorised as an extreme rise in body temperature that can potentially be fatal.
Additionally, the sweat glands can be linked to cystic fibrosis. Eccrine sweat glands usually reabsorb sodium and chloride ions through their ductal epithelium, which causes sweat to be hypotonic. This process is controlled by the hormone aldosterone. However, if defective chloride ion reabsorption occurs, this can lead to parents noticing that a child has salty skin when kissing the child. This acknowledgement leads them to the doctor which usually ends up in a diagnosis of cystic fibrosis. The sweat glands of people with cystic fibrosis appear to be histologically normal, however, they have saltier sweat due to overproduction of sodium and chloride. This issue is related to a protein known as cystic fibrosis transmembrane regulator (CFTR), which is is genetically coded for. Cystic fibrosis a result of a recessive gene meaning that both parents must supply a copy of the defective gene to their child for the disease to occur.
Sources
All content published on Kenhub is reviewed by medical and anatomy experts. The information we provide is grounded on academic literature and peer-reviewed research. Kenhub does not provide medical advice. You can learn more about our content creation and review standards by reading our content quality guidelines.
- Ross, M. H., PhD, & Pawlina, W., MD. (2015). Histology: A Text and Atlas: With Correlated Cell and Molecular Biology (7de editie). Lippincott Williams & Wilkins.
- Mescher, A. (2013). Junqueira’s Basic Histology: Text and Atlas, Thirteenth Edition (13 ed.). McGraw-Hill Education / Medical.
Structure and function of the sweat glands: want to learn more about it?
Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster.
“I would honestly say that Kenhub cut my study time in half.” – Read more. Kim Bengochea, Regis University, Denver
© Unless stated otherwise, all content, including illustrations are exclusive property of Kenhub GmbH, and are protected by German and international copyright laws. All rights reserved.
Register now and grab your free ultimate anatomy study guide!