What glands are ductless and secrete their products?
Recommended readings from Histology, A text and Atlas, M.H. Ross et al, 3rd edition
- Chapter 20 – Endocrine Organs: Disregard information in tables which is not found in the text of this page. Read the text only with the objective of understanding the details mentioned in the lecture notes.
ENDOCRINE GLANDS
Endocrine (or internally secreting) glands are also named ductless glands, since they lack excretory ducts. Instead, the secretory cells release their products, hormones , into the extracellular space. From the extracellular space, the hormones may enter the blood stream, by which they reach their target organs. Alternatively, the hormones may affect nearby cells ( paracrine acting hormones).
The major endocrine glands are the pituitary gland, the pineal body, the thyroid gland, the parathyroid gland, the pancreas, the adrenal glands, the ovaries and the testes. In some of these glands/organs (Which ones?) the endocrine tissue constitutes only part of the parenchyma of the organ. Small groups or individual endocrine cells are also found in a variety of other organs (for example the GIT and the kidneys).
Pituitary Gland
The pituitary gland (or hypophysis) is attached to the inferior surface of the brain by an extension of the nervous tissue of the tuber cinereum /eminentia mediana of the hypothalamus, the infundibulum. The infundibulum and small amounts of non-neural secretory tissue surrounding it form the hypophyseal stalk . The pituitary gland is located in the sella turica, the hypophyseal fossa of the sphenoid bone. The pituitary gland is surrounded by a thin connective tissue capsule. The loose connective tissue between the capsule and the periosteum of the sphenoid bone contains a dense plexus of thin-walled veins, which surround the entire pituitary gland.
Macroscopically, the pituitary gland can be divided into neurohypophysis , which includes all neuroectodemal hypophyseal derivatives, and adenohypophysis , which includes all ectodermal hypophyseal derivatives. Adenohypophyseal tissue extending dorsally along the anterior and lateral surfaces of the hypophyseal stalk is also called pars tuberalis of the hypophysis. The remainder of the adenohypophysis can be divided into a pars intermedia and a pars distalis .
It becomes a little easier to understand the structural divisions of the pituitary gland if you understand the pattern of the development of this gland.
Lab: Any of the pituitary slides available are suitable to look at the general organization of the pituitary. Try also to identify the portal venules (read below). Several of them can usually be seen in the pars tuberalis, where they descend towards the pars distalis of the pituitary. Compare your observations with plate 99 (p.622) in Ross et al .
Draw the pituitary at low magnification and identify its divisions (those visible in the slide) and portal venules on your drawing.
Cells and secretory products of the hypophysis:
Adenohypophysis
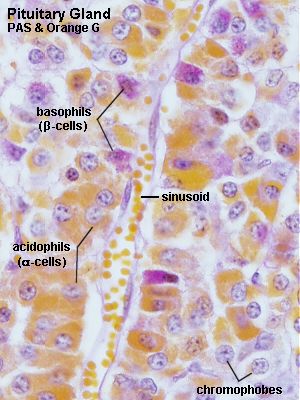
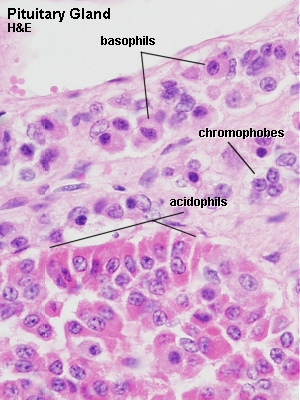
The pars distalis of the adenohypophysis accounts for about 75% of the hypophyseal tissue. The glandular cells are arranged in irregular clumps or cords between a network of capillaries with large and irregular lumina. Connective tissue, which supports the glandular cells, is scant. Traditionally, glandular cells are subdivided into chromophobe cells and acidophil and basophil ( chromophil ) cells . This division into three cell types is based on their differential staining with H&E. Cocktails of other dyes, some of which are mentioned below, also allow a differentiation between these cell types.
All known hormones of the adenohypophysis are proteins or glycoproteins .
The contents of the secretory vesicles are responsible for the staining characteristics of the chromophil cells.
Acidophils are rounded cells and typically smaller than basophil cells. Acidophils account for roughly 65% of the cells in the adenohypophysis.
- The most frequent subtype of acidophils are the somatotrophs (which can be stained with the dye orange G) . Somatotrophs produce g rowth h ormone (GH or somatotropin ), which e.g. stimulates liver cells to produce polypeptide growth factors which stimulate growth � (e.g. somatomedin which stimulates epiphyseal cartilage – overproduction of this hormone may result in gigantism or acromegaly) .
- Mammotrophs (or lactotrophs) , the second group of acidophils, secrete prolactin . Their number increases significantly in late pregnancy and the early months of lactation.
Based on their hormone products basophils are divided into three subtypes.
- Thyrotrophs produce t hyroid s timulating h ormone (TSH or thyrotropin ).
- Gonadotrophs produce f ollicle s timulating h ormone (FSH), which stimulates the seminiferous epithelium in males in addition to early follicular growth in females. Gonadotrophs also produce l uteinizing h ormone (LH), which stimulates production of testosterone by Leydig cells in males in addition to late follicular maturation, oestrogen secretion and formation of corpus luteum in females.
- Corticotrophs (or adrenocorticolipotrophs) secrete a dreno c ortico t ropic h ormone (ACTH or corticotropin ) and lipotropin (LPH, no known function in humans). Corticotropes are the most frequent cell type in the pars intermedia. In the pars intermedia, the precursor of ACTH and LPH undergoes further hydrolysis into m elanocyte s timulating h ormone (MSH , increased pigmentation in patients with Addison’s disease ) and a number of other peptides (among them endogenous opioids).
When stained with the PAS reaction all three types of basophils appear reddish. Morphological criteria may be used, aside from the secretory products, to distinguish between the cells, but differences are so subtle that it is hopeless to try to tell them apart in the available preparations.
Chromophobe cells are unstained or weakly stained cells. Most chromophobe cells can be assigned to the different classes of chromophils if EM and immunocytochemistry are used. They are now thought to represent acidophil and basophilic cells in a dormant or recently degranulated stage (degranulation = release of most of the secretory vesicles) , but may also include stem cells of the secretory cells.
Lab: Slides PITUITARY (SHEEP) H&E, PITUITARY (SHEEP) PAAB+PAS+OG or PITUITARY (SHEEP) PAS+ORANGE G . The best slide to identify the different cell types of the adenohypophysis is the PAS+Orange G stained one. Identify acidophils, basophils and chromophobes. Survey the tissue, and verify that the relative frequencies of the cells are different in different parts of the adenohypophysis.
In the H&E stained sections acidophils are dark pink and basophils look light pink/blue. Staining in the PAAB+PAS+OG section corresponds largely to that in the other PAS+ORANGE G section but the colours are somewhat subdued because of the additional PAAB stain.
Draw part(s) of the adenohypophysis which contains, if possible, all three cell types at high magnification.
The blood supply to the pituitary gland takes on an extraordinary complex form (e.g. confer figure 20.2 in Ross et al .; even this picture is a slight simplification) . At this stage of the course it is important to know that the primary capillary network in the neural part of the hypophyseal stalk drains into 20 or more portal venules , which form a secondary capillary network in the pars distalis of the pituitary gland. The release of hormones from the adenohypophysis is under the control of hormones which are produced by nerve cells in the hypothalamus . For each hormone released by the adenohypophysis there exist release-inhibitory factors and releasing-factors . These factors are also hormones. The axons of hypothalamic nerve cells terminate within the neural stalk and release these regulatory factors into the extracellular space associated with the primary capillary plexus. They are transported towards the adenohypophysis within the portal venules and reach their target cells via the secondary capillary plexus.
Neurohypophysis
Usually only the oval or round nuclei of the pituicytes are visible. Nerve fibres typically terminate close to capillaries. Scattered, large, and bluish-violet masses in the neurohypophysis represent dilation of nerve fibres in which the secretory vesicles, which contain the products of the neurosecretory hypothalamic cells, have accumulated – they are named Herring bodies .
The neurophypophysis expands posterior to the adenohypophysis, where it forms the posterior lobe of the pituitary.
Release-inhibiting and releasing factors are not the only hormones secreted in the neurohypophysis. Oxytocin (contraction of smooth muscle cell in the uterus in late pregnancy, milk ejection reflex) and a nti d iuretic h ormone (ADH or vasopressin ) are secreted in the neurohypophysis in addition to the hormones which regulate the activity of the adenohypophysis.

Lab: Slides PITUITARY (SHEEP) PAAB+PAS+O.G. or PITUITARY (SHEEP) LFB . Identify nuclei of pituicytes and Herring bodies. Herring bodies are not quite as well-defined structures as e.g. Hassal bodies, but rather areas of darker staining in the tissue. You may also want to take a quick look at neurones of the hypothalamus, part of which should be visible on the slides.
Sketch the appearance of the tissue of the neurohypophysis at high magnification and label the structures you can identify.
PINEAL BODY
The pineal body is a flattened, cone-shaped organ attached to the roof of the third ventricle, where it occupies a depression between the superior colliculi.
The pineal body is surrounded by pia mater, which functions as its capsule and which sends connective tissue septae into the pineal body, subdividing it into lobules.
In the pineal we find two cell types: pinealocytes (about 95% of the cells; large, light and round nuclei) and astrocytes (glial cells; dark, elongated nuclei).
Aside from the cells the pineal gland also contains . sand – well – brain sand (or acervuli cerebri or – just for good measure – corpora arenacea) . These are calcium-containing concretions in the pineal parenchyma, which increase in size and number with age. These concretions are radioopaque, and since the pineal is located in the midline of the brain they provide a good midline-marker . They have have no other known function.
The most prominent secretory product of the pineal body is melatonin . The cocktail of substances released by the pinealocytes can have several functions: they may decrease secretory activity in most other endocrine glands (in part indirectly, by way of influencing hypothalamic neurones) , and they may “delay” puberty through antigonadotrophic effects.
Secretory activity in the pineal gland is stimulated by darkness and inhibited by light. Via the effects of pineal hormones on the adenohypophysis and sex hormones it is likely that the pineal body is involved in phenomena associated with the circadian rhythm and seasonal phenomena (e.g. s easonal a ffective d isorder, SAD) . The pineal body is innervated by postganglionic sympathetic fibres derived from the superior cervical ganglion.

Lab: Slide PINEAL GLAND SHEEP H&E . The parenchyma of the pineal gland looks rather homogeneous at low magnification. A few blood vessels are visible criss-crossing through the gland. At higher magnification three types of nuclei can be distinguished. Small dark nuclei belong to the astrocytes found in the pineal gland. Pinealocytes have larger, lighter and round nuclei, which are surrounded by a broad rim of light cytoplasm. Most nuclei present are the nuclei of pinealocytes. Endothelial cell nuclei are found in association with the vessels and capillaries traversing the tissue. Both pinealocytes and astrocytes have long processes which give the tissue between the nuclei its “stringy” appearance.
Brain sand is not visible in this section.
Draw a small part of the parenchyma of the pineal gland at high magnification. Label pinealocytes and astrocytes.
THYROID GLAND
The thyroid gland is situated on the lateral sides of the lower part of the larynx and upper part of the trachea. The two lateral lobes of the thyroid are connected by a narrow isthmus in front of the trachea. The size is quite variable but typically ranges around 20g (slightly larger in females than in males).
The thyroid gland consists almost entirely of rounded cysts, follicles , which are separated by scant interfollicular connective tissue. The follicle is the structural and functional building block of the thyroid gland. It consists of a simple cuboidal epithelium (variable – depending on the functional state) which surrounds a lumen filled with a viscous substance, colloid. The size of the follicles is variable ranging from about 50 µm to about 1 mm.
The colloid is the secretory product of the follicular cell ( extracellular storage! ). Its main component, thyroglobulin , consists of triiodothyronine and tetraiodothyronine (or thyroxine) .
C cells (or parafollicular cells) are part of the follicles. There are only few of them, and they are typically situated basally in the epithelium, without direct contact with the follicular lumen. They are always situated within the basement membrane, which surrounds the entire follicle.
Arterial supply is abundant with a dense network of capillaries between the follicles. Sympathetic fibres (from the superior, middle and inferior cervical ganglia) are mainly vasomotor (there is some evidence that sympathetic input may have a stimulatory effect on secretory activity) .
The main secretory products of the thyroid gland are thyroxine and triiodothyronine. TSH stimulates the endocytosis of thyroglobulin from the follicular lumen and the subsequent release of its components into the blood stream. TSH also stimulates their synthesis and release into the follicular lumen.
These thyroid hormones increase metabolic activity in almost all tissues and organs . Many of the other effects of the hormones are secondary to an increased oxygen consumption of the affected cells and the energy that, as a consequence, becomes available for cellular processes (exceptions to this rule are e.g. effects on lipid metabolism and increases in carbohydrate absorption in the small intestine).
C cells produce the hormone calcitonin , which decreases blood calcium concentration by inhibiting the resorption of bone (primarily by inhibiting osteoclast activity).
Lab: Slide THYROID HUMAN H&E . Identify the follicles of the thyroid gland. Have a look at the height of the epithelium and make an educated guess at the functional activity in the thyroid (well, when it was still alive!) . Notice the capillaries in the interstices between the thyroid follicles. C cells are very difficult to identify.
Pick a nice follicle and draw it.


PARATHYROID GLANDS
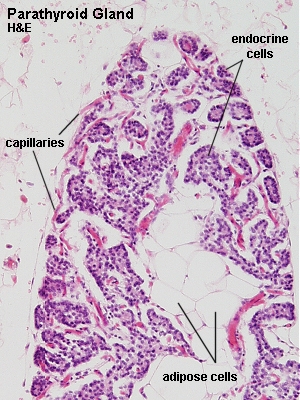
The parathyroid glands are four small oval bodies located at the posterior surface of the thyroid gland (close to the middle and inferior ends of the lateral thyroid lobes – but a bit variable; the inferior pair may actually be located in the mediastinum).
These glands are small (average total weight is about 130 mg – that’s 130 milli grams) but essential for life.
Each parathyroid gland is surrounded by a thin connective tissue capsule. Parenchymal cells are arranged in anastomosing chords surrounded by delicate connective tissue septae. Capillaries are abundant. A considerable number of fat cells infiltrate the gland (beginning around puberty) and may account for about half the weight of the parathyroid glands in adults.
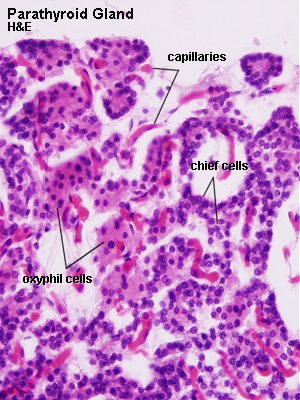
Two cell types can be distinguished in the parathyroid glands:
- Chief cells are the most numerous type. They are rather small, a round, light and centrally placed nucleus and a very weakly acidophilic cytoplasm. They synthesise p ara t hyroid h ormone (PTH or parathormone) which is of pivotal importance for normal calcium concentrations in the fluids and tissues of the body. The effect is mediated by a stimulation of osteoclastic bone resorption, intestinal calcium uptake and calcium resorption in the kidneys. If the parathyroid glands are removed completely, calcium concentrations decrease rapidly, leading to tetany within 2-3 days and eventually death if left untreated.
- Oxyphilic cells are less frequent (entirely lacking in small children; occurring first in children six to seven years old and afterwards increasing in number with age – funny enough they have so far only been demonstrated in Rhesus monkey, the ox and, of course, humans ). Their cytoplasm is strongly acidophilic, the nucleus is small and uniformly intense basophilic. They contain large amounts of mitochondria.
There are plenty of transitional cells, i.e. cells that morphologically represent transitions between chief cells and oxyphilic cells.
Both the release of calcitonin by C cells in the thyroid gland and the release of parathyroid hormone are regulated by negative feedback from blood calcium concentrations.
Lab: Slides PARATHYROID HUMAN H&E or THYROID AND PARATHYROID H&E . Your first task, which may not be that easy,�is to find the parathyroid glands. The glands are small and usually occupy only a small fraction of the tissue on the slide. Give it a good try before you call for help. Identify chief cells and oxyphilic cells.
Draw a part of the tissue in which both cell types are both visible. Include if possible some of the fat cells which may occupy a large part of the parenchyma of the parathyroid.
This slide will not be available in the revision boxes.
ADRENAL GLANDS
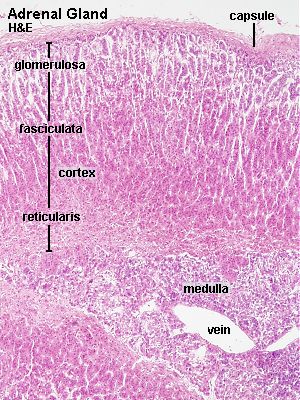
Th adrenal (or suprarenal) glands consist of an outer cortex (the main part of the adrenal glands) and an inner medulla (which accounts for about 10% of the adrenal glands) . The gland is surrounded by a thick connective tissue capsule. Vessels and nerves reach the medulla by way of connective tissue trabeculae which extend from the capsule towards the medulla. Cortex and medulla are two distinct endocrine organs (in lower vertebrates they may actually form two entirely separate organs) .
The cortex is divided into three concentric zones which, from the surface inwards, are termed the zona glomerulosa (accounting for about 15% of the cortical thickness) , the zona fasciculata (about 75%) and the zona reticularis (about 10%) . Transitions are usually gradual.
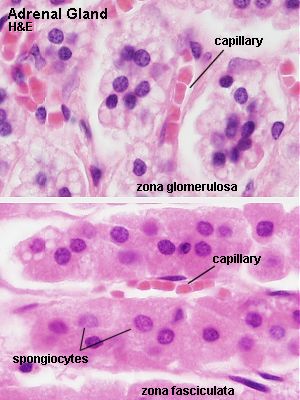
- Cells of the zona glomerulosa are organised into small rounded groups or curved columns. Cells are smaller than in the two other zones, their nuclei are dark and round, and the cytoplasm is light basophilic. The zona glomerulosa is not influenced by ACTH .
- The zona fasciculata consists of radially arranged cell cords separated by fenestrated sinusoid capillaries. The nucleus is light and typically located centrally. The cytoplasm is also light and often has a characteristic foamy or spongy appearance (lipid droplets in the cytoplasm extracted during tissue processing) – they are for this reason also called spongiocytes.
- Anastomosing cell chords separated by sinusoid spaces form the zona reticularis. Cells are typically smaller than in the zona fasciculata. Their cytoplasm is eosinophilic and less spongy than that of other cells in the cortex. The nucleus is rather light and large. Lipofucsin, a pigment, accumulates in the cells with age. These accumulations have an orange tinge in H&E stained preparations.
Both the zona fasciculata and zona reticularis depend on ACTH to sustain their function and survival.
Lab: Slide ADRENAL MKY H&E . Try to find a transect through the adrenal gland where you can see all three zones of the cortex and, if possible, also a bit of the medulla (see below). Note that the relative thickness of the cortical zones may vary. It is not always possible to identify the adrenal medulla beneath the cortex. In addition to chromaffin cells you may find ganglion cells, sometimes in small clusters,�in the medulla. They can be recognized by the “typical” ganglion cell nucleus – LARGE, light and with a distinct nucleolus.
Draw and label a transect of the adrenal gland which contains the three zones and the medulla.

Hormones produced in the cortex are all steroids (consequently, cortical cells contain large amounts of SER and lipids). Since the hormones are synthesised in the cortex they are more precisely termed corticosteroids . Corticosteroids are further subdivided into mineralocorticoids (most important aldosterone ; in renal tubular resorption of sodium, excretion of potassium) and glucocorticoids (most important cortisol ; protein catabolism in almost all cells aside from liver cells, gluconeogenesis, glycogen storage, mobilisation of fat from lipocytes, anti-inflammatory effects, inhibition of allergic reactions ). Small amounts of androgens, oestrogens and progesterone are also produced.
The morphological zonation of the cortex reflects a functional zonation in that
- mineralocorticoids are produced in the zona glomerulosa,
- glucocorticoids are produced in the zona fascicularis and reticularis , and
- sex hormones are produced in the zona reticularis.
The medulla is not sharply delimited from the cortex. Cells are arranged in strands or small clusters with capillaries and venules in the intervening spaces. Their cytoplasm is weakly basophilic. They are called chrom affin cells because the granules of these cells can be stained with potassium bi chrom ate. Chromaffin cells correspond to the adrenaline- (80%) and noradrenaline-containing cells of the medulla. The two groups cannot be distinguished using routine histology. Chromaffin cells are innervated by preganglionic sympathetic fibres and correspond functionally to postganglionic neurones. The correspondence is not only functional – chromaffin cells are , like ganglion cells of the PNS, derived from neural crest cells.
The adrenal medulla is not essential for life.
Page content and construction: Lutz Slomianka
Last updated: 09/01/99