List the endocrine glands
Introduction to endocrine secretion.
Continue on down this page for an overview of several endocrine glands.
Or click on links in this table for pages on each endocrine gland.
INTRODUCTION TO ENDOCRINE SECRETION
Many of the body’s cells secrete substances which influence other cells, either locally or at some distance. Cells which are conspicuously specialized for this function are called endocrine cells. (The suffix -crine refers to secretion; the prefix endo- tells us that the secretory product stays inside the body.) Several additional cell types (e.g., adipocytes, which secrete the hormone leptin) also may have endocrine function but are not traditionally listed with the endocrine organs. Endocrine cells in the endocrine organs listed above all share certain characteristics:
- Most obviously, endocrine cells are all specialized for secretion. Their specific appearance depends on the nature of the secretory product and on the cellular machinery needed to manufacture and store that product.
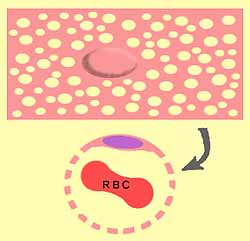
- Secretory products of endocrine cells are secreted into interstitial fluid from whence they can diffuse into blood. Therefore, endocrine secretion does not involve ducts but requires close proximity to blood vessels, usually either capillary networks or vascular sinusoids.
- Endocrine cells are commonly arranged into cords or small clumps, with each cell closely associated with adjacent vessels.
- To faciliate diffusion of hormones into blood, vessels associated with endocrine glands have fenestrated endothelium (from Latin fenestra, window). Each endothelial cell has a shape like a slice of very holey Swiss cheese (cartoon illustration at right), rolled into a cylinder to make a segment of capillary.
The various endocrine cells of the human body are organized in a few distinctive patterns.
EPITHELIAL TISSUE forms the parenchyma of thyroid, parathyroid, anterior pituitary (adenohypophysis), adrenal cortex, pancreatic islets, and liver.
The epithelial nature of these cells is reflected in their organization into cords or clumps, with cells attached laterally to neighboring cells as in surface epithelium. But because there is typically no lumenal surface for endocrine secretion, there is no apical/basal polarization of cytoplasm. (An exception is the thyroid, where proper cuboidal epithelium does form follicles into whose lumens thyroglobulin is secreted for storage.)
With the exception of adrenal cortex (which is mesodermally derived), these glands are all of ectodermal or endodermal origin. Remnants of embryonic origin may occur in the form of displaced glandular tissue or ducts, especially with the adenohypophysis or the thyroid.
NERVOUS TISSUE, derived from neuroectoderm or neural crest, comprises the posterior pituitary (neurohypophysis), adrenal medulla, and pineal.
Both neurohypophysis and pineal originate from the diencephalon and have organization typical of nervous tissue. Secretion is from axon terminals. Secretory cells (neurons) are supported by glial cells.
The adrenal medulla is essentially a sympathetic ganglion originating from neural crest and innervated by preganglionic sympathetic axons. The adrenal medullary cells lack axons but are otherwise functionally similar to sympathetic nerve cells.
CONNECTIVE TISSUE, derived from mesoderm, provides the organizational pattern for testicular Leydig cells, ovarian stromal cells, and for adipose tissue.
OTHER: Ovarian granulosa and luteal cells defy easy tissue-type classification.
Finally, INDIVIDUAL CELLS may have significant endocrine function. Examples include the epithelial enteroendocrine cells of the GI tract and the juxtaglomular cells (modified smooth muscle) of the renal cortex.
Overview of Individual Endocrine Glands
(For additional detail, click on the name of the gland.)The pituitary gland (or hypophysis) consists of two distinct parts, the anterior pituitary (adenohypophysis) and the posterior pituitary (neurohypophysis).
The anterior pituitary appears glandular (hence adenohypophysis), with clumps of epithelial cells with varying staining properties. Cells of several types each secrete one of several hormones (e.g., GH, ACTH, FSH, LH, TSH, etc.) Such secretion from this “master gland” regulates most other endocrine glands and is, in turn, regulated by factors secreted by hypothalamic neurons and delivered to the anterior pituitary by the hypophyseal portal vessels.
The posterior pituitary consists of secretory endings of axons from nerve cells (hence neurohypophysis) whose cell bodies are located in the hypothalamus. These secretory processes of the posterior pituitary secrete oxytocin and ADH.
Pituitary adenomas may be “benign” (i.e., not malignant) but can nevertheless cause significant problems either from excess hormone production or from mass effect (e.g., crowding the optic chiasm). For illustration, see WebPath.
The thyroid consists of characteristic follicles, each with a large lumen surrounded by a simple cuboidal epithelium. The appearance (as well as evolutionary origin) is that of an exocrine gland which has lost its outlet so that secretory product accumulates in the follicles. Follicular cells store thyroglobulin in the follicles for subsequent use in production and endocrine secretion of T3 (thyroxin) and T4. Parafollicular cells (C cells) produce calcitonin.
- For some examples of thyroid pathology, see WebPath (thyroiditis, inflammation), WebPath (Grave’s disease, hyperthyroid), and WebPath (goiter), or Milikowski & Berman’s Color Atlas of Basic Histopathology, pp. 452-461.
The parathyroid consists of several discrete glands, each organized into tangled curvilinear cords of chief cells. These cells secrete parathyroid hormone, which works in opposition to calcitonin (from thyroid C cells) to regulate blood calcium levels.
Pancreatic islets (also called islets of Langerhans (named after Paul Langerhans, b. 1847) are nests of endocrine cells scattered within the pancreas. Each islet consists of several cell types which secrete insulin, glucagon, somatostatin, and pancreatic peptide. The cells are arranged into tangled cords.
- Diabetes may result from immunological destruction of islet cells. For images, see WebPath (diabetes I) and WebPath (diabetes II), or Milikowski & Berman’s Color Atlas of Basic Histopathology, p. 469.
The adrenal consists of two distinct parts, an outer cortex and an inner medulla.
- For images of tumors leading to Cushing’s disease, see WebPath (gross) and WebPath (microscopic), or Milikowski & Berman’s Color Atlas of Basic Histopathology, p. 466.
- For gross images of adrenal hyperplasia (e.g., subsequent to Cushing’s disease or ectopic ACTH production) and also adrenal atrophy, see WebPath
The testis contains clusters of interstitial Leydig cells which secrete testosterone.
The ovary includes steroid secreting cells of the theca interna and of the corpus luteum.
The pineal consists of pinealocytes, neuron-like cells which secrete melatonin. Calcium accumulation (“brain sand”) in the pineal gland makes this structure a useful landmark in x-rays. For images of pineal, as well as more information, see LUMEN or Wikipedia.
Historical note: According to Rene Decartes (1596-1650), it is through the pineal that the soul controls the body.