Hormones and health: a guide to our body’s chemical messengers
Communication is everything. When you send a text message to a friend asking to meet you at a specific place, you are sending a digital signal that you hope will affect your friend’s behaviour. Likewise, communication is everything for our bodies. Our brain needs to send signals throughout the body to control and coordinate actions required to maintain homeostasis and optimal bodily functions.
The endocrine system serves as a communication pathway based on chemical molecules called hormones. Hormones are chemicals released by cells from the endocrine system into the bloodstream to regulate the function of cells and organs in the body. Hormones bind to specific receptors on target cells, triggering a response that affects the function of the cell.
In essence, the endocrine system is a large network of cells and organs located across the body, which is used to release hormones that regulate the function of different organs and cells.
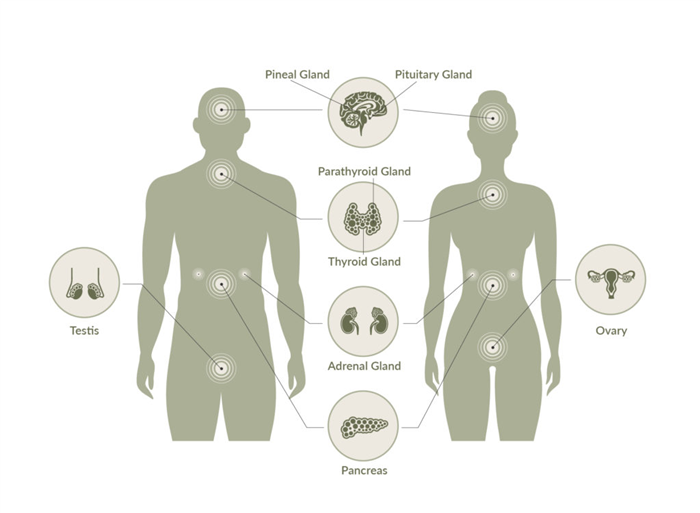
Some key organs forming part of the endocrine system include the adrenal gland, the pituitary and pineal gland, the thyroid glands, the pancreas, and sexual organs. Some of their key functions include:
Hormones produced by the pituitary gland regulate a different aspect of growth and metabolism. Hormones produced by this gland include:
-
- Growth hormone – which regulates growth and physical development, primarily targeting bones and muscles.
- Thyroid-stimulating hormone – which leads to the release of hormones regulating metabolism.
- Adrenocorticotropic hormone – which stimulates adrenal glands to produce cortisol and other hormones.
- Follicle-stimulating hormone – which is involved with estrogen secretion and the growth of egg cells in women and sperm cell production in men.
- Luteinizing hormone – involved in the production of estrogen in women and testosterone in men.
- Prolactin – which helps with milk production in women who are breastfeeding.
- Endorphins and enkephalins – which have pain-relieving properties.
- Beta-melanocyte-stimulating hormone – which helps to stimulate skin pigmentation in response to UV exposure.
- Vasopressin -which helps the body conserve water and prevent dehydration.
- Oxytocin– which stimulates the release of breast milk and stimulates contractions of the uterus during labour.
The pineal gland produces hormones like melatonin, which helps regulate sleep patterns.
From blood glucose levels to regulation of fear, excitement, and pleasure, these hormones are an important part of our physiology.
-
- The thyroid gland produces the hormones T4 (thyroxine) and T3 (triiodothyronine), which help the body produce and regulate other hormones, such as adrenaline (also called epinephrine) and dopamine. These hormones influence behaviours like fear, excitement, and pleasure.
- Hormones produced by the pancreas, such as insulin and glucagon, help regulate glucose levels in the blood.
- Hormones produced by the adrenal glands, such as aldosterone, cortisol and noradrenaline, play different roles in metabolism. Aldosterone, for example, helps control blood pressure by regulating potassium and sodium levels in the body. Cortisol works alongside adrenaline and noradrenaline to help regulate the body’s reaction to stress.
What are our Key Hormones?
From a structural and functional perspective, hormones can be classified as:
These are fat-soluble molecules made from cholesterol. Some key examples of these types of hormones are the three major sex hormones groups: estrogen, androgen and progesterone. These hormones can enter the cell’s nucleus, where they bind to specific receptors and trigger the production of proteins.
These are water-soluble hormones derived from amino acids, such as epinephrine. These hormones bind to protein receptors on the outside surface of the cell. The binding sends a signal to a second messenger molecule inside the cell, which activates enzymes or influences gene expression.
These are hormones composed of long chains of amino acids, up to 200 amino acids long. They include hormones like insulin, growth hormone, and prolactin, and they are stored in endocrine cells until needed to regulate processes like metabolism, lactation, growth and reproduction.
From a functional perspective, some key hormones with important roles in our body include:
Cortisol
Cortisol is a steroid type of hormone made in the adrenal glands and involved with the regulation of metabolism and immune responses, among other functions.
Cortisol helps with your body’s response to stress, regulating immune responses and is involved with the body’s fight or flight response, which is a normal response to perceived threats. Cortisol also controls blood pressure, increases the body’s glucose metabolism, and reduces inflammation and energy levels so that you can take on what your body perceives as a threat.
Altered levels of cortisol can affect the production of other hormones and influence the function of multiple systems in the body. For example, if you are under constant stress, your body will produce high cortisol levels, leading to high blood pressure. It can influence the development of conditions like diabetes, obesity and osteoporosis, as well as affect fertility.
- weight gain, particularly around the abdomen and face
- thin and fragile skin
- acne
- for women, facial hair and irregular menstrual periods
Symptoms of too little cortisol include:
Melatonin
The brain produces melatonin in response to darkness. It helps with the timing of the body’s circadian rhythms (24-hour internal clock) and sleep.
In the pineal gland, a small, pea-shaped gland located in the brain, but it is also produced in other parts of the body. Notably, it is also produced in the gastrointestinal tract, where it can reach high levels. The melatonin levels in the gastrointestinal tract surpass those in the blood by 10-100 times, and there is about 400 times more melatonin in the gastrointestinal tract than in the pineal gland.
Melatonin regulates circadian rhythms, like the sleep-wake rhythm, neuroendocrine rhythms or body temperature cycles through its action on MT1 and MT2 receptors.
Melatonin is a common supplement taken to help improve sleep patterns. Evidence suggests that melatonin is likely effective for people who have trouble falling asleep at normal times and with other sleep disorders. However, excessive melatonin levels can cause drowsiness and a reduced core body temperature and may lead to headaches and fatigue.
Leptin and ghrelin
Leptin and ghrelin are known as the ‘hunger hormones’ these two hormones have a major influence on energy balance. Leptin is involved with the long-term regulation of energy balance, suppressing food intake and inducing weight loss. Ghrelin is a fast-acting hormone involved in meal initiation.
Ghrelin is primarily released in the stomach, whereas leptin is produced by fat cells.
These two hormones are involved with appetite regulation. Ghrelin plays an important role in short-term appetite regulation, whereas leptin controls long-term energy balance and is considered a satiety hormone.
Why it matters : Ghrelin is an important hormone due to its stimulatory effects on food intake, fat deposition and growth hormone release. Recent studies also suggest that:
- Ghrelin regulates glucose homeostasis by inhibiting insulin secretion and regulating gluconeogenesis/glycogenolysis.Ghrelin signalling decreases thermogenesis to regulate energy expenditure.
- Ghrelin improves the survival prognosis of myocardial infarction by reducing sympathetic nerve activity.
- Ghrelin prevents muscle atrophy by inducing muscle differentiation and fusion.
- Ghrelin regulates bone formation and metabolism by modulating the proliferation and differentiation of osteoblasts.
- Ghrelin is also involved in cancer development and metastasis.
Leptin is directly correlated with the amount of body fat, and this hormone, along with its receptors, are considered key regulators of body weight and energy homeostasis. Leptin deficiency is very rare but can happen due to genetic deficiencies, where the body cannot produce leptin. In such cases, the absence of leptin can lead to uncontrolled urges to eat, potentially leading to severe childhood obesity. In addition, leptin deficiency may lead to delayed puberty and impaired immune function.
A decrease in sensitivity to leptin by tissues in our body is called ‘leptin resistance’, a condition that can lead to the development of obesity and metabolic disorders, such as insulin resistance and dyslipidemia. Leptin resistance can occur due to the presence of certain mutations in genes encoding leptin and its receptors, as well as in proteins involved in self-regulation of leptin synthesis and blood-brain barrier permeability.
More broadly, certain factors can influence these leptin and ghrelin levels. For example,
- Acute and chronic sleep restriction can lead to a reduction in levels of leptin and increased levels of ghrelin, as described in this recent paper.
- Another recent study, based in animal models, reported that melatonin and leptin interact in the hypothalamus region of the brain to regulate energy balance. These findings hint at a potential explanation for the high incidence of metabolic diseases observed in individuals exposed to light at night.
- Another important factor involves levels of cortisol. One study found that high levels of cortisol, alongside insulin and chronic stress, were predictions of greater future weight gain. This study also associated high ghrelin levels with higher food cravings.
Estrogen, progesterone, and testosterone
Estrogen is commonly known as a ‘female hormone’ and testosterone as the ‘male hormone’, but both are found in males and females at different levels. In women, estrogen is a key driver of sexual development, working alongside the hormone progesterone to regulate women’s menstrual cycles and the reproductive system’s function. In men, estrogen is involved with optimal sexual function.
- Estrogen – in premenopausal women, estrogen is produced mainly in the ovaries, but in postmenopausal women, the ovaries cease to produce this hormone. Instead, estrogen is produced by several extragonadal sites, such as mesenchymal cells of adipose tissue, including that of the breast, osteoblasts and chondrocytes of bone, the vascular endothelium and aortic smooth muscle cells, and numerous sites in the brain. In men, estrogen is synthesised by Leydig cells and the germ cells found in the testis.
- Progesterone – this hormone is commonly produced by the adrenal cortex and the gonads (ovaries and the testes). Progesterone is also produced by the ovarian corpus luteum during the first ten weeks of pregnancy and by the placenta in later stages.
- Testosterone – this hormone is mainly produced by the gonads, by the Leydig cells in the testes and the ovaries. The adrenal glands also produce small quantities in both sexes.
Sex hormones are mainly involved with sexual development and reproduction as well as in non-reproductive functions. For example,
- Sex hormones are the primary drivers of sexual development.
- Estrogen is the female’s main sexual hormone and has a major role in reproductive and sexual development, including puberty, menstruation, pregnancy, and menopause. Estrogen affects the reproductive tract, the urinary tract, the heart and blood vessels, bones, breasts, skin, hair, mucous membranes, pelvic muscles, and the brain, among other functions.
- Progesterone is involved with developing the lining found in the uterus for a fertilised egg; it regulates menstruation and supports pregnancy.
- Testosterone, in men, regulates sex drive (libido), bone mass, fat distribution, muscle mass, and the production of red blood cells and sperm.
Thyroid hormones
Thyroid hormones are hormones produced by the thyroid gland, anterior pituitary gland, and hypothalamus, which together comprise a self-regulatory circuit called the hypothalamic-pituitary-thyroid axis.
- the thyroid gland produces thyroxine or tetraiodothyronine (T4) and triiodothyronine (T3);
- the hypothalamus produces thyrotropin-releasing hormone (TRH);
- the anterior pituitary gland produces thyroid-stimulating hormone (TSH).
These hormones regulate metabolism, growth, and other bodily functions. For example, as described in this recent review, thyroid hormones:
- Can increase the expression of beta-receptors, leading to increases in heart rate, stroke volume, cardiac output, and contractility.
- Can stimulate the respiratory centres and lead to increased oxygenation due to increased perfusion.
- Can cause increased development of type II muscle fibres.
- Can increase the basal metabolic rate.
- Can induce lipolysis or lipid synthesis.
- Can stimulate the metabolism of carbohydrates.
- Thyroid hormones can induce the catabolism of proteins in high doses.
- In children, thyroid hormones act synergistically with growth hormone and stimulate bone growth.
- Help with the maturation of the brain during development. In adults, it can affect mood.
- Hyperthyroidism can lead to hyperexcitability and irritability
- Hypothyroidism can cause impaired memory, slowed speech, and sleepiness.
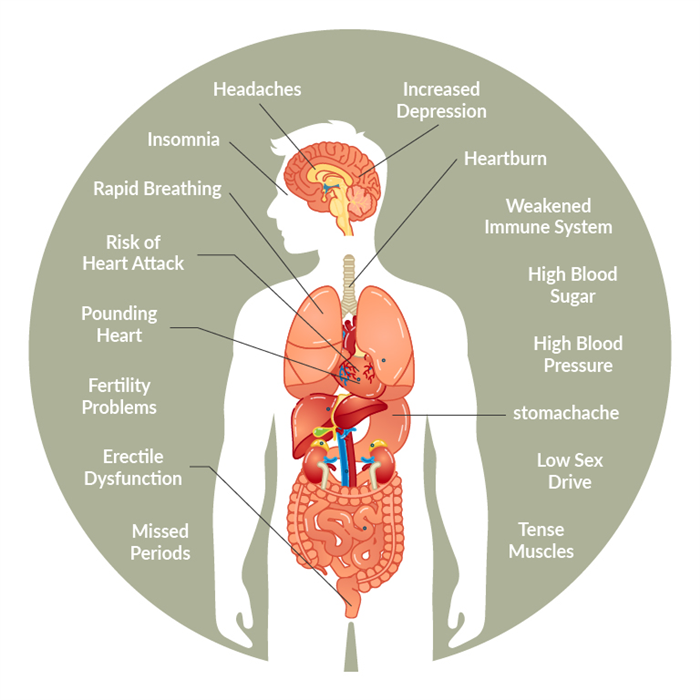
What are common symptoms of hormonal imbalance?
Hormones are needed for virtually every single function in the body. There are over 60 different hormones in the human body, and only when hormone levels are normal is our body functioning at its best. Alterations to the optimal levels of any hormone can significantly affect the body’s function, potentially resulting in adverse health outcomes.
Some symptoms associated with hormonal imbalances include:
- sudden or inexplicable weight gain or weight loss
- difficulty sleeping
- extreme sensitivity to heat or cold
- excessive sweating
- heart rate changes
- dry skin or sudden acne
- anxiety or mood changes
- altered sexual function
- blurred vision
- brittle hair and nails
- excessive hair growth
- breast tenderness
Common causes of hormonal imbalances
Some common causes behind hormonal imbalances involve medical conditions, such as:
- Certain cancers that can reduce estrogen levels
- Cushing’s syndrome or Addison’s disease, which are characterised by too-high or too-low levels of the hormone cortisol, respectively.
- Type 1 and 2 diabetes.
- Hypoglycemia and thyroid disorders.
Beyond medical conditions, injuries, trauma, eating disorders, and stress can lead to hormonal imbalances.
- Stress can lead to changes in blood levels of many hormones, such as glucocorticoids, catecholamines, growth hormone and prolactin. While some of these changes are a normal part of the body’s fight or flight response to danger, they can also lead to endocrine disorders like Graves’ disease, gonadal dysfunction, psychosexual dwarfism and obesity.
- Alcohol – excessive consumption of alcohol disrupts the communication between the nervous, endocrine and immune system. This leads to hormonal disturbances, which affect our body’s physiology, potentially leading to conditions like stress abnormalities, reproductive deficits, body growth defects, thyroid problems, immune dysfunction, cancers, bone disease and psychological and behavioural disorders.
- Processed foods – certain processed foods contain endocrine-disrupting chemicals (EDCs), such as Perfluorochemicals, Bisphenol A (BPA), Phthalates, and Phenol, which can interfere with the normal function of the body’s endocrine system. These EDCs can mimic the structure of hormones or can block their function. Some of these chemicals have been linked to obesity and type 2 diabetes. One review found that frequent consumption of fast foods is linked to fast foods was accompanied by overweight and abdominal fat gain, impaired insulin and glucose homeostasis, lipid and lipoprotein disorders, induction of systemic inflammation and oxidative stress.
Hormones and health at AUSCFM
At AUSCFM, we follow a modern and evidence-based approach to diagnosing and treating pathologies associated with hormonal imbalances. We are on top of current research on hormones’ role in human health. We employ leading diagnostic testing technologies to hormonal imbalances, as well as other markers of health. Our DUTCH hormone test, for example, provides a comprehensive assessment of key hormones and metabolites. This test informs clinicians about key physiological aspects of your body, such as cortisol and melatonin function, levels of dehydroepiandrosterone, cortisol metabolites, six organic acids and levels of sex hormones. To learn more about the DUTCH hormone test, see our article.
Based on our DUTCH hormone test results, we can identify evidence of hormonal imbalances that may be driving your symptoms. The results of this test, for example, can reveal an altered function of the HPA axis. The Hypothalamic-pituitary-adrenal (HPA) axis is part of the endocrine system and a key regulator of homeostatic processes, influencing immune function and our stress response. To learn more about the HPA axis, see our recent article.
In addition to hormone health, we employ advanced testing that targets six additional gut pathologies. Taken together, the results of these seven tests will give us a comprehensive view of the factors influencing a patient’s health and will help us design personalised treatment strategies.
In parallel, getting an in-depth understanding of your current health and lifestyle, including the diet you follow, can help clinicians identify the root of your problems. Working closely with your practitioner and health coach, you can resolve the underlying cause of hormone imbalance with a personalised plan, including changes to your nutrition, lifestyle, and stress management practices.