24 hours in the life of a hormone: what time is the right time for a pituitary function test?
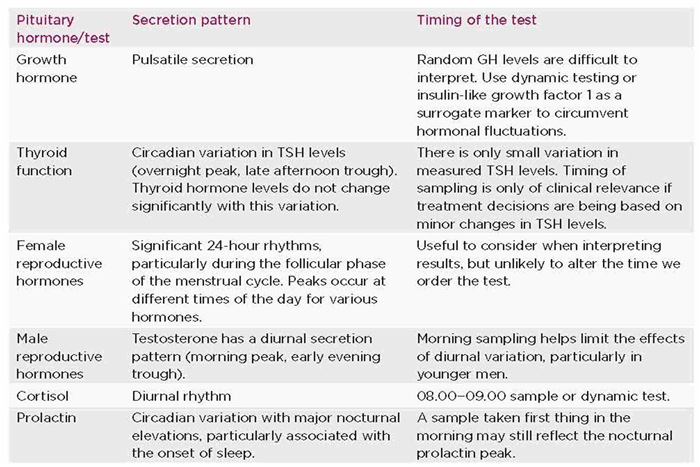
The pulsatile nature and rhythmic pattern of hormone secretion can have important implications for the measurement of circulating hormone levels.
As many hospitals in the UK migrate to electronic patient records and ordering systems, it is all too easy to click on pre-ordered pathology panels, and not pause to consider what is actually being requested. Pathology tests taken at the wrong time of day waste resources, cause inconvenience and can provoke anxiety for health professionals and patients alike when trying to interpret unhelpful results.
Having an understanding of the pattern of pituitary hormone secretion will guide us in determining the optimal time to order these investigations. Here, I summarise issues relating to some common endocrine blood tests, to serve as a reminder to ‘think before we click’ when ordering tests.
GROWTH HORMONE
Generally, ordering a random growth hormone (GH) level is unhelpful; the results will be difficult to interpret. Frequent blood-sampling techniques have demonstrated the pulsatile nature of GH secretion, with approximately eight peaks per 24-hour period, predominately at night. Between pulses, the serum GH concentration may be undetectable. 1
Numerous other endogenous and exogenous factors (e.g. age, sex, weight, sleep, food, stress and exercise) influence the complex regulatory mechanism of the GH axis. 2,3 Given that 5- to 20-minute sampling for 24 hours is not practical, we usually rely on dynamic testing to investigate GH excess (oral glucose tolerance test) or deficiency (e.g. insulin tolerance test or glucagon stress test).
THYROID FUNCTION TESTS
The timing of phlebotomy is not usually considered when ordering thyroid function tests. Circadian variation in thyroid-stimulating hormone (TSH) levels has been well described, with secretion partially pulsatile and partially basal. TSH concentrations are maximal overnight and lowest in the late afternoon to early evening. 4,5 Despite this, thyroid hormone levels do not rise significantly after an overnight TSH surge, possibly because overnight TSH molecules are less bioactive than those circulating in the day. 6
A TSH measurement at 09.00 has been shown to strongly correlate with the total 24-hour TSH secretion, sampled at 10-minute intervals. 7 The circadian differences in secretion may cause a small variation in TSH levels − in older literature a mean of 0.95−2 mIU/l − although generally this does not result in TSH values outside the normal reference range. 8
Thus, the timing of a TSH sample may only be of relevance if treatment decisions are being based on minor changes in TSH level.
FEMALE REPRODUCTIVE HORMONES
The fluctuations of female reproductive hormones within a single day are not usually considered when interpreting test results, but these hormones do exhibit endogenous circadian regulation. Oestradiol, progesterone, follicle-stimulating hormone (FSH) and luteinising hormone (LH) show significant 24-hour rhythms during the follicular phase of the menstrual cycle. In contrast, only FSH is significantly rhythmic during the luteal phase. The hormonal peaks have been found to occur in the morning for progesterone, in the afternoon for FSH and LH, and during the night for oestradiol. 9
These findings are unlikely to alter the time of day we order female reproductive hormone measurements. However, they are useful to consider when interpreting test results alongside factors we regularly take into account, such menstrual cycle phase or menopausal status.
TESTOSTERONE
Testosterone secretion has a diurnal pattern of secretion. Peak levels are reached in the morning between 07.00 and 10.00, a trough is seen in the evening and levels then begin to rise again at night. 10 One study found young men (30–40 years old) to have average 08.00 testosterone levels (both free and total) that were 30–35% higher than levels measured in the mid- to late afternoon. This difference declined with age, dropping to approximately 10% at 70 years of age. 11 This blunting of the circadian rhythmicity of testosterone with normal ageing has been well described. 12
Sampling testosterone in the morning may limit the effects of diurnal variation, and current recommendations are to check a 08.00−09.00 testosterone level, along with sex hormone-binding globulin.
In terms of monitoring testosterone replacement, it depends on the product used. Recommendations from the product information sheet vary from clinical recommendations. For example, product sheets suggest checking testosterone levels pre-application for Testogel® and Testim®, and 2 hours after application for Tostran®. In clinical practice, it is often advised to check testosterone concentration 4–6 hours after application.
CORTISOL
It is well known that cortisol has a circadian rhythm, with levels peaking in the morning between 08.00 and 09.00, and smaller secondary peaks after meals. 13,14 This diurnal rhythm can be affected by sleep and working night shifts.
Since the advent of the newer cortisol assays, we often see a low afternoon cortisol, and endocrinologists are frequently asked to assess hypothalamic-pituitary-adrenal (HPA) function. There is good concordance with 09.00 cortisol as a starter to define HPA function, which is why we generally advise standardised 09.00 cortisol measurement first off. 15 However, if this does not yield an answer, it may be necessary to move to stimulatory tests, such as a synacthen test or insulin tolerance test.
PROLACTIN
When interpreting a single sample showing a mildly raised prolactin level, we often take into consideration external factors (such stress or certain medications), but rarely the diurnal variation of prolactin secretion.
Prolactin is secreted in a circadian and pulsatile pattern with major nocturnal elevations. Sleep onset is rapidly followed by an increase in prolactin secretion, and awakenings coincide with an immediate offset of secretion. 16,17 Hence, the highest levels occur in the early hours of the morning. A sample taken first thing in the morning may still reflect the nocturnal prolactin peak, and repeating the sample later in the day may yield a different result.
Anneke Graf, Department of Endocrinology, University College London Hospitals NHS Foundation Trust
REFERENCES
- Plotkick LP et al. 1975 Journal of Clinical Endocrinology & Metabolism40 240−247.
- Veldheis JD et al. 2008 Endocrine Reviews29 823−864.
- Murray PG et al. 2015 Journal of Endocrinology226 T123−T140.
- Brabant G et al. 1990 Journal of Clinical Endocrinology & Metabolism70 403–409.
- Ehrenkranz J et al. 2015 Thyroid25 954–961.
- Persani L et al. 1995 Journal of Clinical Endocrinology & Metabolism80 2722−2728.
- Roelfsema F et al. 2014 Journal of Clinical Endocrinology & Metabolism99 570−578.
- Keffer JH 1996 Clinical Chemistry42 125−134.
- Rahman SA et al. 2019 Journal of Clinical Endocrinology & Metabolism104 6049−6059.
- Gall H et al. 1979 Andrologia11 287−92.
- Brambilla DJ et al. 2009 Journal of Clinical Endocrinology & Metabolism94 907–913.
- Plymate SR et al. 1989 Journal of Andrology10 366−371.
- Newell-Price J et al. 2008 Clinical Endocrinology68 130−135.
- Bhake RC et al. 2019 Journal of Clinical Endocrinology & Metabolism104 5935−5947.
- Mackenzie SD et al. 2019 Clinical Endocrinology91 608−615.
- Spiegel K et al. 1994 Sleep17 20−27.
- Saleem M et al. 2018 Clinical Biochemist Reviews39 3−16.