The Thyroid Gland
The thyroid gland is an endocrine structure located in the neck. It plays a key role in regulating the metabolic rate of the body.
In this article, we shall look at the anatomy of the thyroid gland – its position, blood supply, and clinical correlations.
Anatomical Location
The thyroid gland is located in the anterior neck and spans the C5-T1 vertebrae. It consists of two lobes (left and right), which are connected by a central isthmus anteriorly – this produces a butterfly-shape appearance.
The lobes of the thyroid gland are wrapped around the cricoid cartilage and superior rings of the trachea. The gland is located within the visceral compartment of the neck (along with the trachea, oesophagus and pharynx). This compartment is bound by the pretracheal fascia.
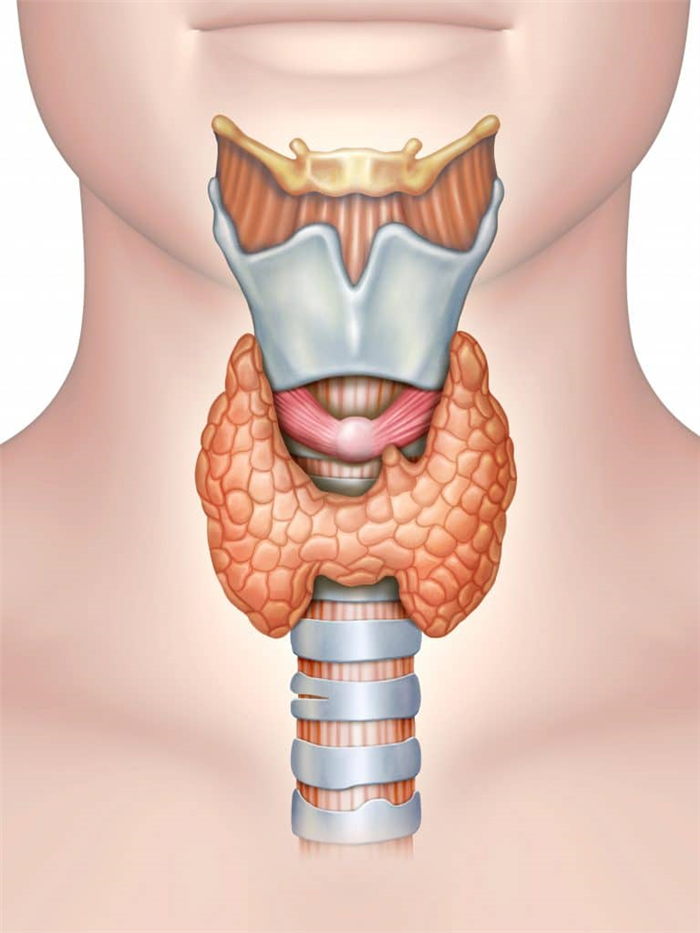
Fig 1 – Overview of the position of the thyroid gland in the neck
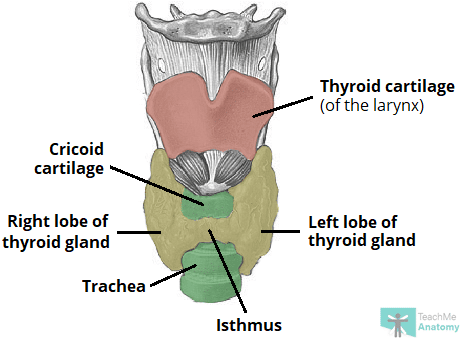
Fig 2 – The thyroid gland consists of two lobes connected by a central isthmus. It is wrapped around the cricoid cartilage and trachea anteriorly.
Clinical Relevance: Thyroglossal Cyst
In the embryo, the thyroid gland begins development near the base of the tongue – in an area known as the foramen cecum. It descends during development and reaches its destination in the anterior neck by week 7.
The descent of the developing thyroid gland forms the thyroglossal duct – an epithelialised tract that connects the gland to its origin at the foramen cecum. It usually regresses by the 10th week of gestation, but can persist in some individuals. If it fails to regress, the duct can give rise to cysts or fistulae.
A thyroglossal cyst results from a build-up of secretions within the duct. It typically presents as a midline lump in the anterior neck which rises on tongue protrusion. If left untreated, this cyst can become infected, and form a cutaneous fistula – discharging out onto the skin of the anterior neck.
Thyroglossal cysts and fistulae are usually treated with complete excision. Recurrence is quoted at approximately 2.5%.
Anatomical Relations
The thyroid gland is closely associated with numerous other structures in the anterior neck:
- Anteriorly – infrahyoid muscles, namely the sternothyroid, superior belly of the omohyoid and sternohyoid
- Laterally – carotid sheath, containing the common carotid artey, internal jugular vein and vagus nerve
- Medially –
- Organs – larynx, pharynx, trachea and oesophagus
- Nerves – external laryngeal and recurrent laryngeal
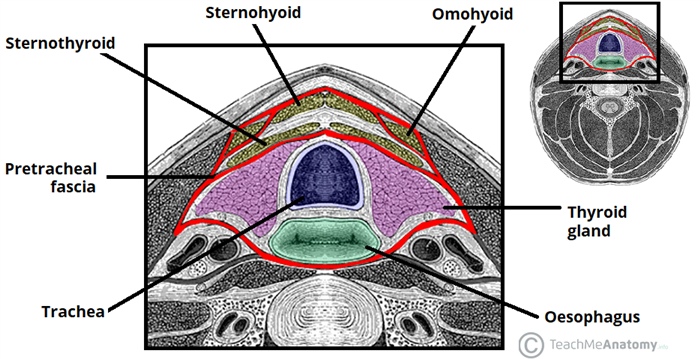
Fig 3 – Transverse section of the neck, showing the pretracheal fascia in red.
Vasculature
The thyroid gland secretes hormones directly into the circulation and is highly vascularised.
Arterial Supply
The arterial supply to the thyroid gland is via two main arteries:
- Superior thyroid artery – arises as the first branch of the external carotid artery. It lies in close proximity to the external branch of the superior laryngeal nerve (innervates the larynx).
- Inferior thyroid artery – arises from the thyrocervical trunk (a branch of the subclavian artery). It lies in close proximity to the recurrent laryngeal nerve (innervates the larynx).
In a small proportion of people (around 10%) there is an additional artery present – the thyroid ima artery. It arises from the brachiocephalic trunk and supplies the anterior surface and isthmus of the thyroid gland.
Venous Drainage
Venous drainage is carried by the superior, middle, and inferior thyroid veins, which form a venous plexus around the thyroid gland.
The superior and middle veins drain into the internal jugular vein and the inferior empties into the brachiocephalic vein.
Innervation
The thyroid gland is innervated by branches derived from the sympathetic trunk.
These nerves do not control the secretory function of the gland – the release of thyroid hormones is regulated by the pituitary gland.
Lymphatic Drainage
The lymphatic drainage of the thyroid is to the paratracheal and deep cervical nodes.
Clinical Relevance: Recurrent Laryngeal Nerve
The left and right recurrent laryngeal nerves lie in close proximity to the thyroid gland and care must be taken not to damage them during thyroid surgery.
They branch from their respective vagus nerve within the chest and hook around the right subclavian artery (right RL nerve), or the arch of aorta (left RL nerve).
The recurrent laryngeal nerve then travels back up the neck, running between the trachea and oesophagus in the tracheoesophageal groove. It then passes underneath the thyroid gland to innervate the larynx.
- Interactive 3D Models
- Access over 1700 multiple choice questions
- Advert Free
- Custom Quiz Builder
- Performance tracking
The thyroid gland is an endocrine structure located in the neck. It plays a key role in regulating the metabolic rate of the body.
In this article, we shall look at the anatomy of the thyroid gland – its position, blood supply, and clinical correlations.
Anatomical Location
The thyroid gland is located in the anterior neck and spans the C5-T1 vertebrae. It consists of two lobes (left and right), which are connected by a central isthmus anteriorly – this produces a butterfly-shape appearance.
The lobes of the thyroid gland are wrapped around the cricoid cartilage and superior rings of the trachea. The gland is located within the visceral compartment of the neck (along with the trachea, oesophagus and pharynx). This compartment is bound by the pretracheal fascia.
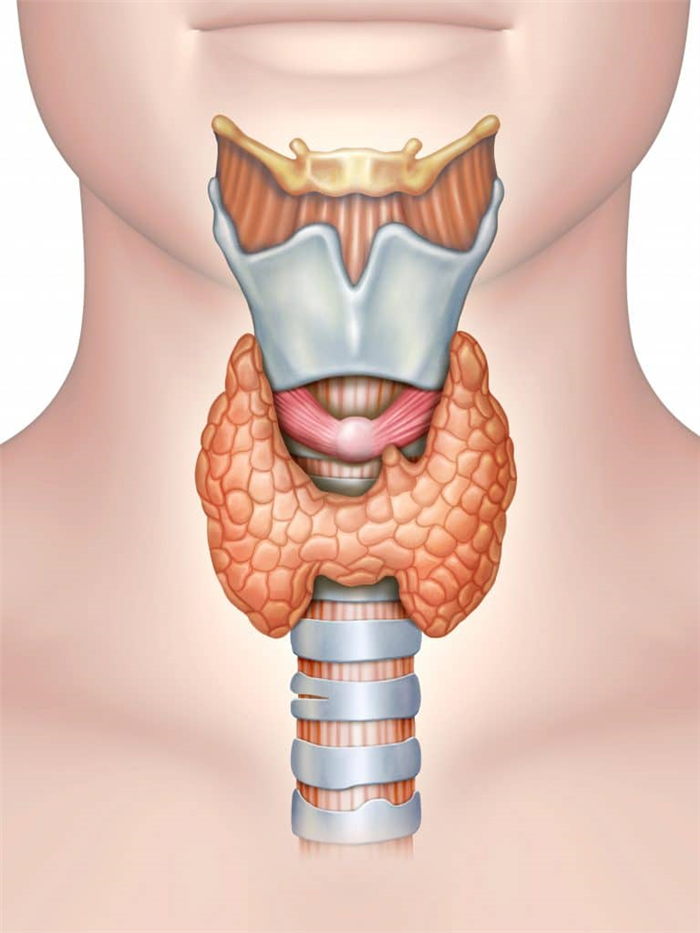
Fig 1 – Overview of the position of the thyroid gland in the neck[/caption]
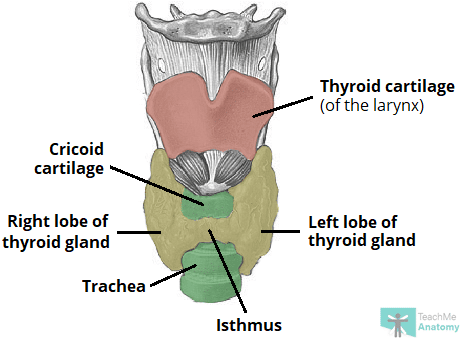
Fig 2 – The thyroid gland consists of two lobes connected by a central isthmus. It is wrapped around the cricoid cartilage and trachea anteriorly.[/caption]
Clinical Relevance: Thyroglossal Cyst
In the embryo, the thyroid gland begins development near the base of the tongue – in an area known as the foramen cecum. It descends during development and reaches its destination in the anterior neck by week 7.
The descent of the developing thyroid gland forms the thyroglossal duct – an epithelialised tract that connects the gland to its origin at the foramen cecum. It usually regresses by the 10th week of gestation, but can persist in some individuals. If it fails to regress, the duct can give rise to cysts or fistulae.
A thyroglossal cyst results from a build-up of secretions within the duct. It typically presents as a midline lump in the anterior neck which rises on tongue protrusion. If left untreated, this cyst can become infected, and form a cutaneous fistula – discharging out onto the skin of the anterior neck.
Thyroglossal cysts and fistulae are usually treated with complete excision. Recurrence is quoted at approximately 2.5%.
Anatomical Relations
The thyroid gland is closely associated with numerous other structures in the anterior neck:
- Anteriorly – infrahyoid muscles, namely the sternothyroid, superior belly of the omohyoid and sternohyoid
- Laterally – carotid sheath, containing the common carotid artey, internal jugular vein and vagus nerve
- Medially –
- Organs – larynx, pharynx, trachea and oesophagus
- Nerves – external laryngeal and recurrent laryngeal
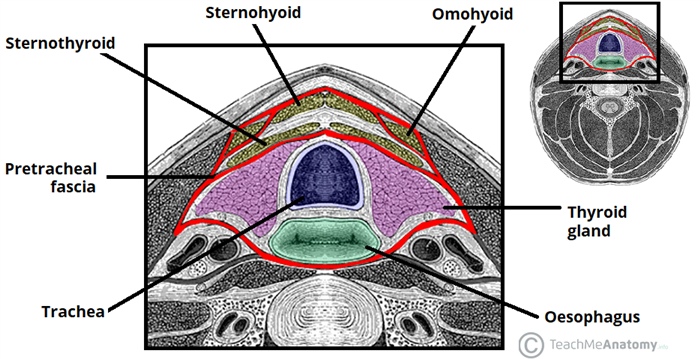
Fig 3 – Transverse section of the neck, showing the pretracheal fascia in red.[/caption]
Vasculature
The thyroid gland secretes hormones directly into the circulation and is highly vascularised.
Arterial Supply
The arterial supply to the thyroid gland is via two main arteries:
- Superior thyroid artery – arises as the first branch of the external carotid artery. It lies in close proximity to the external branch of the superior laryngeal nerve (innervates the larynx).
- Inferior thyroid artery – arises from the thyrocervical trunk (a branch of the subclavian artery). It lies in close proximity to the recurrent laryngeal nerve (innervates the larynx).
In a small proportion of people (around 10%) there is an additional artery present – the thyroid ima artery. It arises from the brachiocephalic trunk and supplies the anterior surface and isthmus of the thyroid gland.
Venous Drainage
Venous drainage is carried by the superior, middle, and inferior thyroid veins, which form a venous plexus around the thyroid gland.
The superior and middle veins drain into the internal jugular vein and the inferior empties into the brachiocephalic vein.
Innervation
The thyroid gland is innervated by branches derived from the sympathetic trunk.
These nerves do not control the secretory function of the gland – the release of thyroid hormones is regulated by the pituitary gland.
Lymphatic Drainage
The lymphatic drainage of the thyroid is to the paratracheal and deep cervical nodes.
Clinical Relevance: Recurrent Laryngeal Nerve
The left and right recurrent laryngeal nerves lie in close proximity to the thyroid gland and care must be taken not to damage them during thyroid surgery.
They branch from their respective vagus nerve within the chest and hook around the right subclavian artery (right RL nerve), or the arch of aorta (left RL nerve).
The recurrent laryngeal nerve then travels back up the neck, running between the trachea and oesophagus in the tracheoesophageal groove. It then passes underneath the thyroid gland to innervate the larynx.